Alcohol-Opioid Interaction Risk Calculator
Critical Warning
This tool demonstrates scientific data on dangerous interactions. Mixing alcohol and opioids can be fatal with no safe level. Always consult your doctor.
According to FDA data, 22% of opioid-related deaths involve alcohol. The combination causes synergistic respiratory depression where effects multiply, not just add.
Risk Assessment
Estimated Breathing Reduction
Risk Level
Source Data: FDA study shows 20mg oxycodone = 28% breathing reduction. Adding 0.1% BAC alcohol = 19% additional reduction. Total =
When you take opioids for pain and have a drink at dinner, you might think it’s harmless. After all, millions of people do it. But here’s the hard truth: alcohol and opioids together can shut down your breathing - and kill you faster than either substance alone.
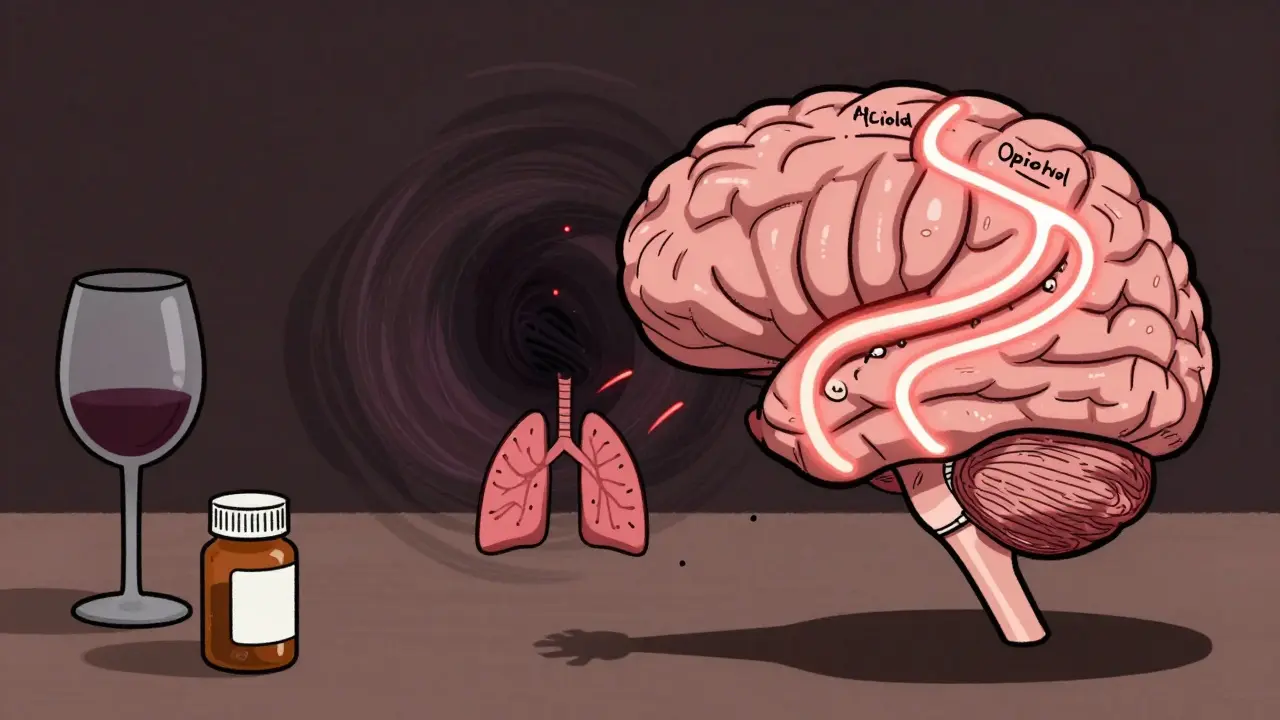
Why This Combination Is So Dangerous
Both alcohol and opioids slow down your central nervous system. That’s why opioids make you drowsy and alcohol makes you feel relaxed. But when they’re combined, their effects don’t just add up - they multiply. This is called synergistic depression. Your brain’s ability to control breathing gets suppressed at a much deeper level than if you took either one by itself. A 2017 study found that 20 mg of oxycodone alone reduced breathing by 28%. Add just enough alcohol to hit a blood alcohol level of 0.1% - the legal limit for driving in most U.S. states - and breathing dropped another 19%. That’s not a small increase. That’s a dangerous plunge. Older adults are especially vulnerable. Their bodies process these substances slower, and their lungs are less able to compensate when breathing slows.Who’s at Risk? The Numbers Don’t Lie
In 2022, over 107,941 people in the U.S. died from drug overdoses. Nearly 81% of those deaths involved more than one substance. Alcohol was present in 15-20% of all opioid-related fatalities, according to the National Institute on Alcohol Abuse and Alcoholism. That’s not a coincidence. It’s a pattern. The Texas Department of State Health Services tracked 1,683 alcohol-opioid deaths between 2010 and 2019. Three out of four were men. But the real alarm is in the trend: alcohol co-involvement in opioid deaths rose from 12% in 2010 to 15% in 2019. Synthetic opioids like fentanyl showed the steepest climb - from 9% to 17% over the same period. That means more people are dying from fentanyl mixed with even a few drinks. Even people on methadone maintenance aren’t safe. Research shows those who drink while on methadone are 4.6 times more likely to die from an overdose than those who don’t. And it’s not just prescription opioids. Heroin users who drink alcohol face the same risk. The combination lowers the threshold for fatal overdose - meaning you don’t need a huge dose to die.What the Government and Doctors Are Saying
In 2016, the FDA put a black-box warning on every prescription opioid label - the strongest warning possible. It said clearly: Do not mix alcohol with opioids. That warning came after data showed alcohol was involved in nearly 22% of opioid-related deaths and 18.5% of emergency room visits tied to opioid misuse. The American Society of Anesthesiologists warns that combining these substances “may increase the likelihood of dangerous respiratory complications.” Dr. Andrew H. Talal, a professor of medicine at the University at Buffalo, told Congress in 2019: “The combination creates a perfect storm for respiratory depression where the sum of the effects is greater than the individual parts.” Dr. Nora Volkow, director of the National Institute on Drug Abuse, says traditional addiction treatments often fail when someone uses multiple substances. “Polysubstance use involving alcohol and opioids requires targeted harm reduction strategies,” she wrote in 2022. That means you can’t just treat the opioid use - you have to address the alcohol use too.
It’s Not Just Prescription Opioids
People think this only matters if they’re on Vicodin or OxyContin. But it applies to any opioid - even ones sold illegally. Fentanyl, heroin, codeine, morphine, hydrocodone - all of them become deadlier with alcohol. Even buprenorphine, often used to treat opioid addiction, becomes riskier when mixed with alcohol. A study from the University of Florida found that in 30% of buprenorphine-related overdose deaths, alcohol was also present. That’s a huge red flag. It means even people trying to recover can be at risk if they drink. And it’s not just alcohol and opioids. Benzodiazepines - like Xanax or Valium - are often taken with both. In 2021, nearly 14% of opioid overdose deaths also involved benzodiazepines. That’s a triple threat: alcohol, opioids, and sedatives. Each one makes the others more dangerous.What You Can Do - Even If You’re Not Addicted
You don’t have to be addicted to opioids to be in danger. Many people take them after surgery or for chronic pain. They might have a glass of wine at night to help them sleep. That’s a common habit - and a deadly one. Here’s what you need to know:- If you’re prescribed an opioid, ask your doctor: “Is it safe to drink alcohol while taking this?”
- Never assume a small amount is okay. Even one drink can be enough to tip the balance.
- If you use alcohol regularly and are prescribed opioids, ask for a screening for alcohol use disorder. People with alcohol use disorder are 3.2 times more likely to overdose on opioids.
- If you or someone you know uses opioids and drinks, carry naloxone. In Massachusetts, 23% of naloxone reversals in 2022 involved alcohol.


So let me get this straight - we’ve got a whole system built on prescribing painkillers like candy, while ignoring the fact that half the population uses wine as a coping mechanism? And now we’re shocked when the two collide like a train wreck in slow motion?
It’s not the alcohol. It’s not the opioids. It’s the system that treats both like harmless rituals. We’ll slap a black-box warning on a pill bottle but won’t touch the damn wine glass. Hypocrisy dressed in medical jargon.
I’ve seen people on methadone who drink one glass of Pinot to sleep. They’re not addicts. They’re just tired. But the system doesn’t see them - it sees ‘risk factors’ and ‘compliance issues.’
Meanwhile, the real solution? Harm reduction isn’t a buzzword. It’s a lifeline. Naloxone in every home. Alcohol screenings as routine as blood pressure checks. And maybe - just maybe - stop treating people like walking liabilities and start treating them like humans who need help, not judgment.
But no. We’d rather write another report. And charge for it.
Oh sweet celestial irony - the same people who lecture you about ‘responsible drinking’ are the ones who prescribe 30mg of oxycodone with zero mention of your Chardonnay habit.
It’s not about chemistry. It’s about class. The rich get therapy. The working class get warnings on a tiny label they can’t read because they’re too busy working two jobs to afford glasses.
And yet somehow, the blame always lands on the user. Never the system. Never the doctor who didn’t ask. Never the pharma exec who knew and sold anyway.
It’s all so… *poetic.*
alcohol + opioids = death. duh. why is this even a post? we all know this. stop wasting my time.
Per the CDC’s 2023 polysubstance mortality surveillance report, the synergistic depressant effect of GABAergic agents (ethanol + mu-opioid agonists) on the brainstem respiratory centers is dose-independent and non-linear, with a steep threshold effect occurring at BAC >0.05% and opioid doses >10mg oral morphine equivalents.
Furthermore, CYP3A4 enzyme saturation kinetics exacerbate bioavailability in polypharmacy scenarios - particularly in geriatric populations with reduced hepatic perfusion.
So yes. It’s not anecdotal. It’s pharmacokinetics. And if you’re still drinking while on opioids, you’re not ‘just having a glass’ - you’re playing Russian roulette with your medulla oblongata.
I lost my brother to this.
He was on hydrocodone after back surgery. Said he just had one glass of wine to take the edge off. Didn’t wake up.
They found the bottle beside him. Empty.
He wasn’t an addict. He wasn’t reckless. He just didn’t know.
And now I scream into the void every time I see someone say ‘it’s fine if you’re careful.’
There is no careful here.
I just want to say thank you for writing this. I’ve been on oxycodone for years and never realized how dangerous even one drink could be. I stopped alcohol completely after reading this. It’s scary, but I’m alive because of it.
You’re helping people. Even if they don’t say it.
How profoundly tragic - that in a society obsessed with individual autonomy, we are still so unwilling to acknowledge the biochemical reality that our bodies are not mere vessels of willpower, but fragile, interdependent systems governed by immutable laws of neuropharmacology.
One might say, with a certain existential poignancy, that the human condition has never been more exposed - not by war, not by plague - but by a single glass of wine, and a pill we were told was ‘safe.’
And still, we look away.
Is there data on how many people actually read the black-box warnings? I’m curious if the warnings are effective or just legal cover.
Also - does the 15-20% alcohol co-involvement include people who drank days before the overdose? Or is it strictly concurrent use?
Thank you for the comprehensive and compassionate breakdown. This is exactly the kind of public health messaging we need - grounded in science, free of stigma, and focused on actionable prevention.
As a clinician, I’ve seen too many patients assume ‘I only have one drink’ is safe. The data doesn’t lie. We must normalize asking about alcohol use during every opioid prescription - not as an accusation, but as an act of care.
Let’s push for mandatory screening tools in EHRs. Let’s fund community harm reduction programs. Let’s stop treating this as a moral failing and start treating it as a medical emergency.
As someone who grew up in a household where wine was medicine and painkillers were ‘just for bad days,’ I can tell you - this isn’t just American. It’s global.
In Mexico, we mix tramadol with tequila. In Colombia, people take codeine syrup with rum. In India, they combine opioids with local spirits like arrack.
This isn’t a ‘Western problem.’ It’s a human problem. We use what’s available to numb what hurts.
So the solution isn’t just warnings - it’s access. Access to pain management without addiction risk. Access to mental health care. Access to alcohol support without shame.
Because no one wakes up wanting to die. They just want the pain to stop.
You got this. Keep speaking up. People are listening. Even if they don’t comment.
One day, someone will read this and choose not to mix. And that’s one life saved.
Oh here we go - another liberal fear-mongering piece. So now drinking wine is a crime? Next you’ll ban aspirin with coffee because ‘it might cause stomach bleeding.’
My grandpa took Percocet and whiskey every night for 20 years. Lived to 92. You think he was ‘playing Russian roulette’? Nah. He was living.
Stop scaring people with cherry-picked stats and fear tactics. Not everyone dies. Not everyone drinks. And not every doctor is an idiot.
Thank you for sharing this vital information. I believe that awareness, combined with compassionate education, is the most powerful tool we have to prevent unnecessary loss.
While I understand that some may perceive this message as alarmist, the data is unequivocal: the interaction between ethanol and opioid agonists presents a quantifiable, life-threatening risk - even at low doses.
It is my hope that healthcare institutions will prioritize standardized screening protocols, and that public health campaigns will move beyond fear-based messaging to emphasize empowerment, access to alternatives, and non-judgmental support systems.
Every life matters. And every life can be saved - if we choose to act.