Anticholinergic Burden Calculator
Assess Your Medication Risk
This tool estimates your cumulative anticholinergic burden based on your medications and usage duration. Long-term use of strong anticholinergics may increase dementia risk by nearly 50%.
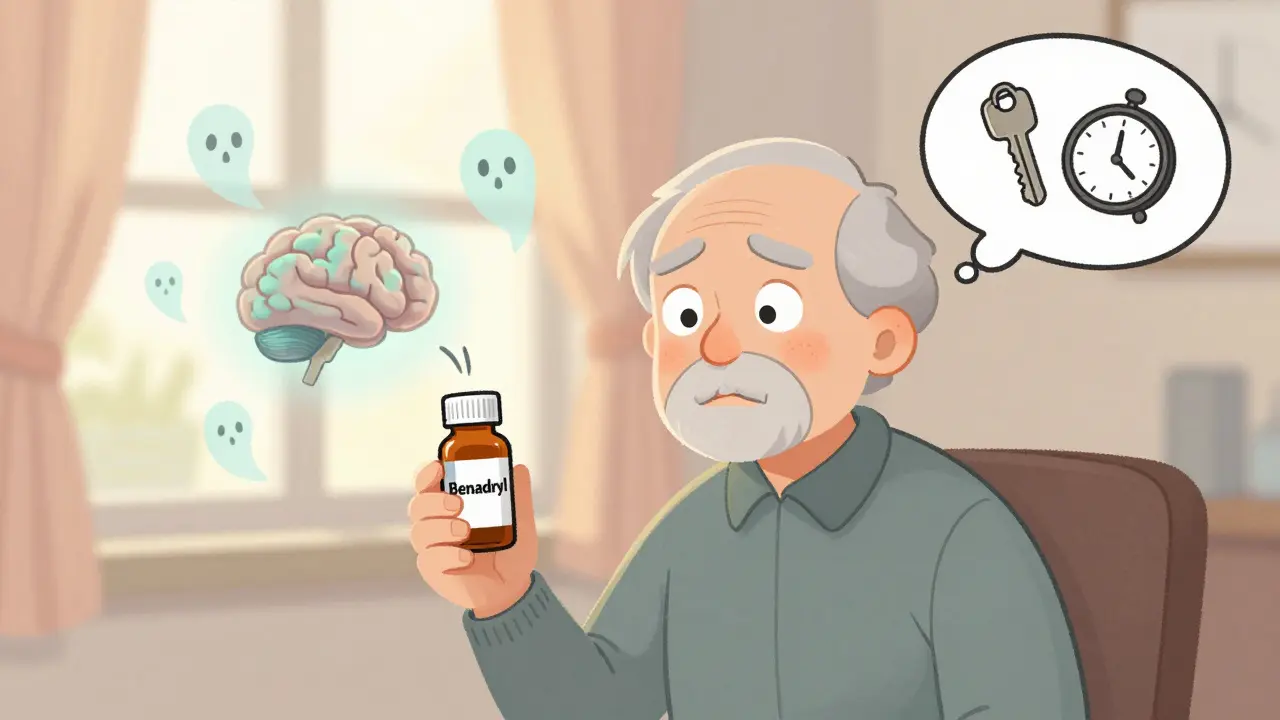
Many older adults take medications for common issues like allergies, overactive bladder, depression, or insomnia-drugs like Benadryl, oxybutynin, or amitriptyline. What most people don’t realize is that these commonly prescribed or over-the-counter pills may be quietly increasing their risk of dementia. The link isn’t theoretical. It’s backed by years of brain scans, population studies, and real-world data showing that long-term use of anticholinergic drugs is tied to measurable memory loss and faster brain shrinkage.
What Are Anticholinergic Medications?
Anticholinergic medications block acetylcholine, a chemical in your brain and body that helps nerves communicate. This can help with things like reducing muscle spasms, drying up excess saliva or sweat, or calming an overactive bladder. But when acetylcholine is blocked in the brain, it interferes with memory, attention, and thinking.
There are about 100 medications with anticholinergic effects. Common ones include:
- Diphenhydramine (Benadryl, Advil PM, Tylenol PM)
- Oxybutynin (Ditropan) and Solifenacin (Vesicare) for overactive bladder
- Amitriptyline and other tricyclic antidepressants
- Chlorpheniramine (in many cold and allergy meds)
- Hydroxyzine (for anxiety or itching)
Some of these are available without a prescription. That’s part of the problem. People don’t think of Benadryl as a drug that could hurt their brain-they think of it as a sleep aid or allergy pill. But it’s one of the most common sources of anticholinergic exposure in seniors.
How Much Risk Are We Talking About?
It’s not about taking one pill. The danger builds up over time. A 2019 study using data from over 3,400 people found that those who took medications with strong anticholinergic effects for more than three years had a 49% higher risk of developing dementia compared to those who didn’t take them at all.
That number might sound shocking, but here’s what it looks like in real terms:
- People taking just 1-90 total daily doses (about 3-4 months) saw a 6% increased risk.
- At 100-900 doses (roughly a year), the risk jumped to 18%.
- After 900+ doses (over three years), it hit nearly 50%.
Brain imaging studies show why. People on these drugs had 0.5% to 1.2% more annual brain volume loss in areas like the hippocampus-the part responsible for memory. Their brains also showed 4-8% lower glucose metabolism, meaning brain cells weren’t getting enough energy to function properly. These changes look a lot like early signs of Alzheimer’s disease.
Not All Anticholinergics Are the Same
Here’s something critical: not all these drugs carry the same risk. Some are far worse than others.
According to a 2019 study in JAMA Internal Medicine, the highest risk comes from:
- Antidepressants (especially tricyclics like amitriptyline)-1.29 times higher dementia risk
- Antipsychotics-1.20 times higher risk
- Bladder drugs like oxybutynin and solifenacin-1.13 to 1.23 times higher risk
- Antiparkinson drugs-slightly elevated risk
But not all bladder medications are equal. Trospium, another drug for overactive bladder, showed no increased dementia risk in the same study. Why? Because it doesn’t cross the blood-brain barrier as easily. That’s a big deal. Drugs that stay out of the brain are safer for your thinking skills.
Similarly, newer antihistamines like loratadine (Claritin) or cetirizine (Zyrtec) have minimal anticholinergic effects. They’re much better choices than diphenhydramine for allergies or sleep.
Real People, Real Consequences
Stories from patients tell a clearer picture than statistics alone.
One Reddit user shared that their mother took amitriptyline for eight years for nerve pain. Her memory test score (MMSE) dropped from 28 to 22-clear signs of cognitive decline. After stopping the drug, her score stabilized, but never returned to normal. Another person on the Alzheimer’s Association forum reported clearer thinking and better focus after switching from oxybutynin to mirabegron, a non-anticholinergic bladder drug.
But here’s the gap: on Drugs.com, 68% of users rated oxybutynin as “excellent” or “good” for bladder control. Only 22% mentioned memory problems. Why? Because the side effects are slow. People don’t connect forgetting where they put their keys or struggling to find the right word with the pill they’ve been taking for years.
And doctors? A 2021 survey found only 37% of primary care physicians routinely check for anticholinergic burden in patients over 65-even though nearly 90% know it’s a risk. That’s a disconnect between science and practice.
What Can You Do?
You don’t have to stop all medications overnight. But you can take smart steps.
- Review your meds with your doctor. Bring a full list-prescriptions, OTCs, supplements. Ask: “Is this drug anticholinergic? Is there a safer alternative?”
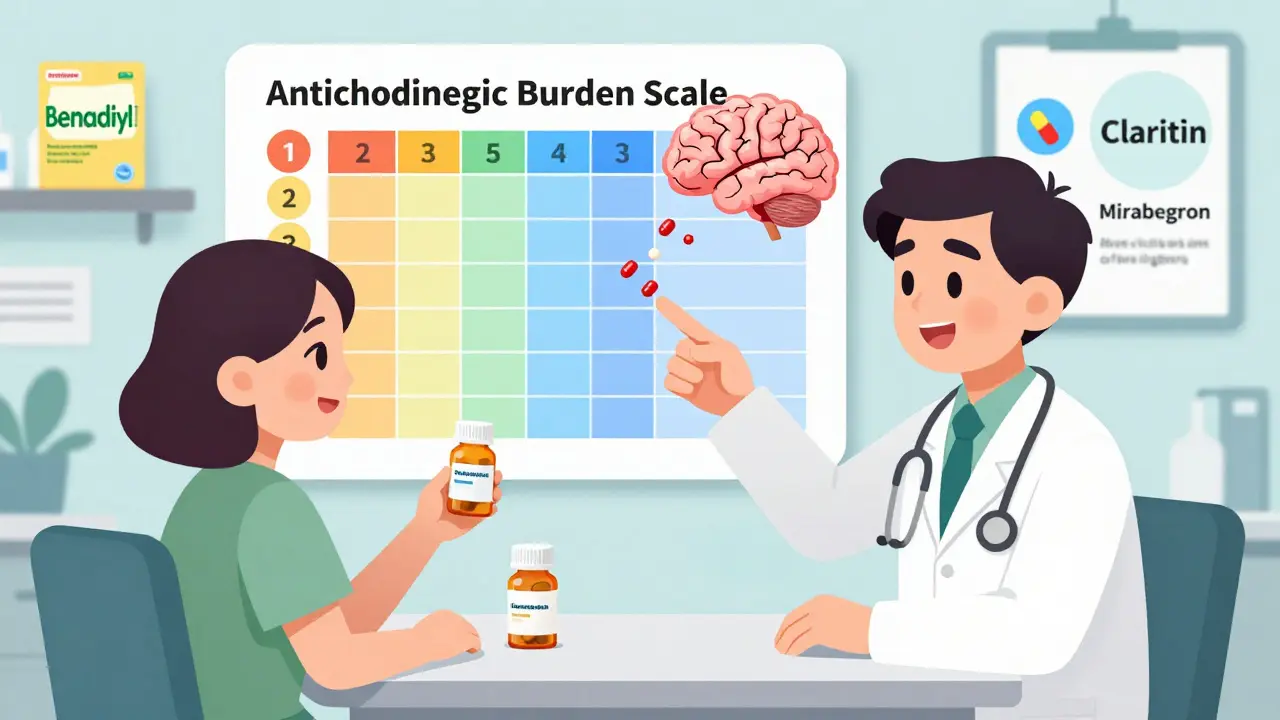
- Check the ACB scale. The Anticholinergic Cognitive Burden scale ranks drugs from 1 (mild) to 3 (strong). Avoid anything rated 3 if you’re over 65 or have memory concerns.
- Switch when possible. For allergies: use loratadine instead of diphenhydramine. For bladder issues: try mirabegron or non-drug options like pelvic floor therapy. For depression: SSRIs like sertraline have little to no anticholinergic effect.
- Don’t quit cold turkey. Stopping some anticholinergics suddenly can cause withdrawal-nausea, sweating, heart racing. Tapering over 4-8 weeks is safer.
Some pharmacies now have anticholinergic burden calculators built into their systems. Ask your pharmacist to run a check. It takes less than a minute.
What’s Being Done?
Major health organizations are acting. The American Geriatrics Society updated its Beers Criteria in 2019 to say: avoid strong anticholinergics in older adults. The FDA added stronger warning labels to 14 drugs in 2020. The European Medicines Agency restricted several bladder drugs for elderly use in 2021.
Research is moving forward too. The PREPARE trial, launched in 2022, is following 3,000 people who carry a genetic risk for Alzheimer’s. They’re stopping anticholinergics to see if it delays dementia onset. Early results aren’t out yet, but the trial itself shows how seriously this is being taken.
Drug companies are responding. As of mid-2023, at least seven new bladder medications and three new antidepressants are in late-stage trials-all designed to avoid crossing into the brain. That’s a $1.3 billion market shift toward safer options.
Bottom Line
Anticholinergic medications aren’t evil. They help people with real, often painful conditions. But when used long-term in older adults, they can quietly damage the brain. The risk isn’t guaranteed-it’s cumulative. And it’s preventable.
If you or a loved one is taking one of these drugs, don’t panic. But do ask questions. Talk to your doctor. Look for alternatives. Even small changes-like switching from Benadryl to Claritin-can make a difference over time.
Memory loss isn’t always aging. Sometimes, it’s a side effect of a pill you didn’t realize could hurt your brain.
Can anticholinergic medications cause permanent memory loss?
Some people experience lasting cognitive changes after long-term use, especially if they’ve taken high-burden drugs like amitriptyline or oxybutynin for several years. Brain scans show structural changes, and memory tests often don’t fully recover even after stopping the medication. But not everyone is affected the same way. Early detection and discontinuation may prevent or limit damage.
Is it safe to take Benadryl occasionally for sleep?
Taking diphenhydramine once in a while-like once a month-is unlikely to cause harm. But using it regularly, even just a few nights a week, adds up. For older adults, even occasional use can contribute to confusion or falls. Safer sleep options include melatonin, cognitive behavioral therapy for insomnia, or non-anticholinergic sleep aids like doxylamine (used cautiously).
What are the best alternatives to oxybutynin for overactive bladder?
Mirabegron (Myrbetriq) is the top alternative-it works differently and has no anticholinergic effect. Other options include tolterodine (lower risk than oxybutynin), or non-drug approaches like bladder training, pelvic floor exercises, or timed voiding. Some people benefit from Botox injections into the bladder, which have no cognitive side effects.
How do I know if a medication is anticholinergic?
Check the Anticholinergic Cognitive Burden (ACB) scale online or ask your pharmacist. Common anticholinergics include any drug ending in “-dine” (like diphenhydramine), “-onin” (oxybutynin), or tricyclic antidepressants. The ACB scale rates drugs from 1 to 3-avoid anything rated 3, especially if you’re over 65.
Are there any benefits to taking anticholinergics that outweigh the risks?
Yes-for some people, these drugs are essential. Someone with severe Parkinson’s may need them to control tremors. A person with chronic, debilitating overactive bladder might not respond to alternatives. The key is not to avoid them entirely, but to use them only when necessary, at the lowest dose, and for the shortest time possible-with regular check-ins about cognitive health.
If you’re concerned about memory changes, start by reviewing your medications. You might be surprised how many common pills are quietly affecting your brain. A simple conversation with your doctor could lead to a switch that protects your thinking skills for years to come.

I used to take Benadryl every night like it was candy. Didn’t think twice. Now my mom’s forgetting her own birthday. 😔 Maybe it’s not just aging after all.
This is why Indians dont get dementia we dont take all these western pills
My grandma switched from oxybutynin to mirabegron and she’s been her old self again. I wish we’d known sooner.
So let me get this straight… we’re told to avoid anticholinergics, but the FDA still lets companies sell them like candy? Classic.
This is all fearmongering. My uncle took amitriptyline for 20 years and he’s still out there golfing at 82. Your brain’s not a lightbulb that burns out from one pill.
i just found out my zyrtec is safe but my advil pm is a brain killer?? wait i thought zyrtec was the one that made me sleepy?? 🤯
I checked my meds on the ACB scale and holy crap I’ve got three level 3s 😳 I’m calling my doctor tomorrow. Thanks for the wake-up call 🙏
People who don’t read labels deserve what they get. If you’re popping Benadryl like it’s candy and then complaining about memory loss, stop blaming the medicine and start blaming yourself.
I work with seniors every day, and I’ve seen this over and over. One woman stopped her tricyclic antidepressant and started walking her dog again-she hadn’t done that in years. It’s not magic. It’s neurochemistry. And yes, it’s reversible in many cases if caught early. Please don’t wait until your grandkids have to help you find your glasses. Talk to your doctor. Ask for alternatives. You’re not weak for wanting to keep your mind sharp-you’re wise.
You know what’s worse than anticholinergics? The fact that Big Pharma doesn’t want you to know this. They make billions off these drugs. And now they’re pushing ‘safe’ alternatives that cost 10x more. It’s not about your brain-it’s about profit. 🤑 But hey, at least the FDA added a warning… after 40 years of ignoring the science.
I took oxybutynin for 5 years. My memory got so bad I forgot my wife’s birthday. I switched to mirabegron. Now I remember everything. Even her favorite flower. I cried when I realized I’d been poisoning myself.
I’m not saying this isn’t real, but let’s not turn every little memory lapse into a medical crisis. I forget where I put my keys every day. It’s called being human. Not every pill is a villain. Some of us need these meds to function. Balance, people. Balance.