Introduction to Atazanavir and its Importance in HIV Care
As a blogger who has dedicated my life to understanding and sharing information about HIV treatment, I cannot stress enough the importance of medical ethics in HIV care. In this article, I will be discussing Atazanavir, an essential antiretroviral medication used in the treatment of HIV, and the role of medical ethics in HIV care. My goal is to educate and inform readers about the importance of Atazanavir and the ethical considerations that come into play in the treatment of HIV patients.
What is Atazanavir and How Does it Work?
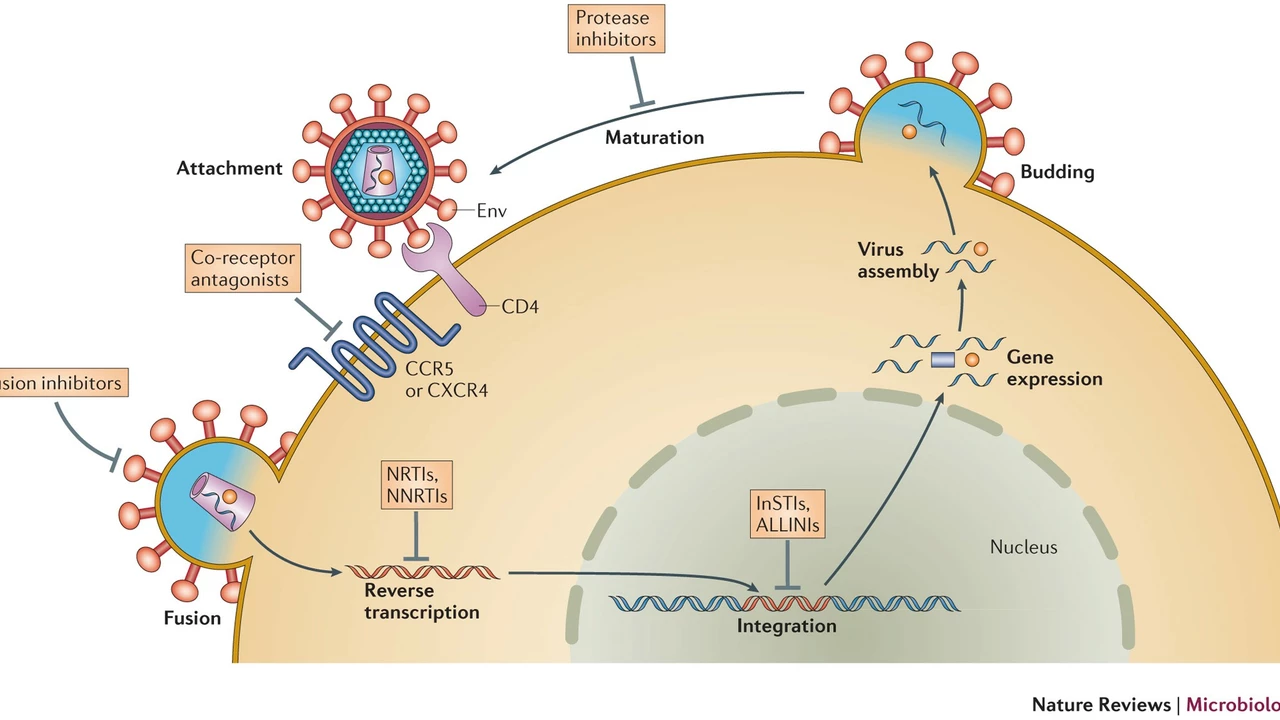
Atazanavir is a protease inhibitor used in combination with other antiretroviral drugs for the treatment of HIV. Protease inhibitors work by blocking the action of an enzyme called HIV protease, which is responsible for the replication of the virus. By inhibiting the protease enzyme, Atazanavir prevents the virus from multiplying and infecting new cells. This helps to slow down the progression of the disease and allows the immune system to recover.
Atazanavir is usually taken once daily and is often prescribed as a part of a complete HIV treatment regimen, which typically includes two other antiretroviral drugs. It is important to note that while Atazanavir can effectively lower the viral load in the body, it cannot cure HIV. However, when taken as prescribed, it can help individuals with HIV lead healthier and longer lives.
Medical Ethics in HIV Care: Patient Confidentiality
One of the most critical aspects of medical ethics in HIV care is patient confidentiality. Due to the stigma associated with HIV, it is crucial for healthcare providers to maintain the utmost privacy when it comes to their patients' diagnosis and treatment. This means that all personal and medical information must be kept confidential, and any disclosure of such information should only occur with the patient's consent.
Respecting patient confidentiality not only protects the individual's privacy but also encourages them to seek medical care and adhere to their treatment plan without fear of discrimination or judgment. Furthermore, it helps to reduce the spread of the virus by ensuring that individuals feel comfortable accessing HIV testing, counseling, and treatment services.
The Ethical Dilemma of Cost and Accessibility
Another critical aspect of medical ethics in HIV care is the dilemma of cost and accessibility. Atazanavir, like many other antiretroviral medications, can be quite expensive, especially in low and middle-income countries where the majority of people living with HIV reside. This raises the question of whether it is ethically acceptable to prioritize the treatment of some individuals over others based on their ability to afford the medication.
Many organizations and initiatives are working to improve access to affordable HIV medications, including Atazanavir, for those who need them most. Ensuring that all individuals living with HIV have access to life-saving treatment is not only a matter of medical ethics but also a crucial step in ending the global HIV epidemic.
Ensuring Informed Consent in HIV Treatment Decisions
Another essential aspect of medical ethics in HIV care is ensuring informed consent. This means that healthcare providers must provide patients with comprehensive information about their treatment options, including the benefits, risks, and potential side effects of each medication. In the case of Atazanavir, it is crucial for patients to be aware of the potential risks associated with the drug, such as liver problems and the possible need for regular blood tests to monitor their liver function.
By providing patients with all the necessary information, healthcare providers empower them to make informed decisions about their own treatment, which is a fundamental ethical principle in medical care. It is also important to respect patients' autonomy and support their decisions, even if they choose not to pursue a particular treatment option.
Addressing the Stigma Surrounding HIV
As a blogger and advocate for HIV care, I believe that addressing the stigma surrounding HIV is a crucial aspect of medical ethics. Stigma can have a detrimental effect on individuals living with HIV, causing them to feel isolated, discriminated against, and less likely to access essential healthcare services. This, in turn, can negatively impact their overall health and well-being, as well as contribute to the spread of the virus.
Healthcare providers have an ethical responsibility to challenge and combat the stigma surrounding HIV by providing accurate information about the virus, promoting understanding and empathy, and treating all patients with respect and dignity. This will ultimately lead to better patient outcomes and help to reduce the global burden of HIV.
Conclusion: The Importance of Medical Ethics in HIV Care
In conclusion, the role of medical ethics in HIV care cannot be overstated. By ensuring patient confidentiality, providing informed consent, addressing cost and accessibility issues, and combating stigma, healthcare providers can create a more just and inclusive healthcare system for individuals living with HIV. As a blogger, I am committed to raising awareness about the importance of medical ethics in HIV care and the life-changing impact that medications like Atazanavir can have on those affected by this virus.

Ah, the lofty ideal of medical ethics in HIV care, a realm where philosophers could lose a few brain cells to bureaucracy. Atazanavir, that protease inhibitor, is hailed as a miracle while its price tag screams capitalistic charity. One could argue that the very notion of confidentiality is a relic, preserved only for those who can afford a private room. The ethical dilemma of cost, of course, is just another episode of “who gets to live when the cash register rings.” In a world where liver enzymes are monitored like stock prices, informed consent becomes a polite formality rather than a genuine dialogue. The stigma attached to HIV is a social virus that spreads faster than the pathogen itself, feeding on ignorance and prejudice. While clinicians parade around with pamphlets on autonomy, the real power lies in who can sign a check. The idea that a single pill can “empower” patients is as naïve as believing a unicorn exists. Moreover, the push for accessibility often masquerades as altruism while ignoring the structural inequities baked into pharmaceutical patents. One must also consider the paradox that a drug designed to suppress a virus may itself suppress hope when priced beyond reach. Governments, NGOs, and profit‑driven companies engage in a delicate dance, each stepping on the toes of the other, all under the banner of “ethical responsibility.” The notion of “informed” consent evaporates when the patient cannot afford the medication they were told about. All of this, wrapped in the comforting language of patient rights, is a charming illusion. So, dear reader, keep your expectations low and your sarcasm high, because the reality of Atazanavir is a textbook case of ethics meeting economics.
Let’s cut through the jargon and recognize that Atazanavir’s efficacy isn’t a myth, it’s a well‑documented fact 😊. However, the cost barrier feels like a velvet rope at a club-only the privileged get in. Confidentiality, when truly respected, becomes a shield that encourages people to seek testing without fear of gossip. In low‑income settings, the ethical conundrum isn’t just about privacy; it’s about whether the drug will ever reach the shelves. We need more cooperative pricing models, not just rhetorical applause for “patient autonomy”.
Honestly, the whole “ethics” buzz is just a marketing ploy for pharma.
Reading about Atazanavir’s promise feels like a distant echo when my clinic’s budget hits a wall. I see patients' eyes dim as they hear “we can’t afford it”. The silence that follows is louder than any lecture on confidentiality.
It’s infuriating that society pretends to care about HIV patients while turning a blind eye to the price tags that keep life‑saving drugs out of reach. This hypocrisy is a moral failing that should shame every decision‑maker who puts profit above people.
Atazanavir works well but the cost issue remains a stark reminder of market failures.
Imagine a world where every HIV‑positive individual could access Atazanavir without worrying about their bank account. That vision isn’t utopian; it’s a realistic goal if governments and companies collaborate creatively. Let’s champion policies that prioritize health over profit.
What most people don’t realize is that the “high cost” narrative is carefully crafted by a hidden alliance of pharma giants and lobbyists. They profit from our fear of the virus while pretending to champion ethics. The real cure lies in transparency, not in the shadows of corporate greed.
There are promising initiatives already lowering Atazanavir prices in several regions, proving that collective effort can overcome barriers. Stay hopeful and support organizations pushing for affordable treatment; every small win counts.
Oh, the glorious march toward justice!; Yet, we must not forget the countless souls still trapped by red‑tape and exorbitant fees; Each policy triumph is a beacon, but the darkness remains, demanding relentless vigilance; Let us raise our voices, louder than ever, and shatter the chains of inequity!;
Indeed, the drama of progress is real, but sustained change requires practical steps-negotiated pricing, generic production, and community advocacy. Let’s channel the passion into actionable plans.