When you walk into a pharmacy in Australia and pick up your prescription, you might pay just $7.70-or $31.60-if you’re not eligible for a concession. That low price isn’t luck. It’s the result of one of the most powerful public health systems in the world: the Pharmaceutical Benefits Scheme (PBS). The PBS doesn’t just make medicine affordable. It shapes the entire market for generic drugs in Australia, forcing prices down, encouraging competition, and sometimes creating unintended roadblocks for patients who need the latest treatments.
Since 1948, the PBS has been the backbone of Australia’s drug access system. It doesn’t give out free medicine. Instead, it pays most of the bill. For every prescription filled, the government covers about 90% of the cost. Patients pay the rest-unless they hit the safety net. That safety net kicks in after $1,571.70 in out-of-pocket spending in 2025. After that, concession card holders pay just $7.70 per script. General patients pay $31.60. Starting January 1, 2026, that number drops to $25. That’s not a minor tweak. It’s a $784 million savings for patients over four years.
But here’s what most people don’t realize: the PBS doesn’t just set prices. It controls how generics enter the market. In 2024, generics made up 84% of all prescriptions filled under the PBS-but only 22% of the total spending. Why? Because even though there are more generic pills out there, the original brand-name drugs still cost way more. The PBS uses a system called reference pricing to fix that. If five drugs treat the same condition, the government picks the cheapest one as the benchmark. All the others get priced to match-or they get pushed out. That’s why generic statins, for example, now make up 95% of the market within 18 months of a patent expiring. No other country does this as aggressively.
How the PBS Decides What Gets Listed
Not every drug that’s approved in Australia gets subsidized. The Pharmaceutical Benefits Advisory Committee (PBAC) decides what makes the cut. They don’t just look at whether a drug works. They ask: Is it worth the cost? The PBAC uses a rough rule of thumb: if a drug costs more than AU$50,000 per quality-adjusted life year (QALY), it’s probably not worth listing. But that’s not a hard limit. Some rare disease drugs cost over AU$150,000 per QALY and still get approved under the Highly Specialised Drugs Program (HSDP). That’s because the PBAC considers how badly patients need it-life expectancy, severity, and whether there are any alternatives.
Still, the system is slow. On average, it takes 587 days from when a drug is launched globally to when it’s listed on the PBS. In Germany? 320 days. In Canada? 410. That gap means Australian patients often pay thousands out-of-pocket while waiting. One study found people with newly approved cancer drugs spent an average of $1,850 during that waiting period. For many, that’s more than a month’s rent.
The Generic Market: Who Wins, Who Loses
The top five generic manufacturers-Symbion, Sigma, Mylan, Aspen, and Hospira-control nearly 70% of Australia’s generic market. They’ve built their businesses around the PBS rules. When a brand-name drug loses patent protection, these companies rush in with cheaper versions. The PBS then slashes the reference price. After six months, the generic price drops to 60% of the original. After a year, it drops again to 43%. That forces manufacturers to compete on price, not marketing.
The result? In cardiovascular drugs, the average price of a generic falls by 74% within a year of multiple entries. In CNS drugs, it’s 68%. That’s why Australia’s generic market is bigger than the OECD average. But not all drugs behave the same. Biologics-complex, injectable medicines for things like rheumatoid arthritis or Crohn’s disease-don’t follow the same rules. Because they’re harder to copy, generics (called biosimilars) take longer to enter. And even when they do, the PBS doesn’t always treat them as true substitutes. That’s why only 63% of the biologic market is now made up of generics, compared to 95% for statins.
Who’s Really Affected?
For people with concession cards-seniors, low-income earners, people on disability-the PBS is a lifeline. One in five Australians has a concession card. For them, a 60-day supply of five medications costs just $7.70. No monthly bills. No tough choices.
But for those without? It’s different. A 2024 national health survey found 12.3% of general patients-about 1.8 million people-skipped doses or didn’t fill prescriptions because of cost. That’s not a small number. One Reddit user, ‘MedicareWarrior,’ wrote: “I’m a self-funded retiree. Five prescriptions a month at $31.60 each? That’s $158. I’m choosing between medicine and groceries.” That’s not an outlier. A 2025 report from the Australian Council of Social Service found 28% of low-income households with chronic conditions cut back on food to afford meds.
Pharmacists feel the pressure too. On average, they handle 17.3 PBS-related transactions per day. Nearly 70% say authority-required prescriptions-those needing special approval-slow them down. One pharmacist told me: “I’ve got a patient who needs a drug that’s on the PBS, but the form takes three days to process. They’re in pain. I can’t give them the medicine until the system catches up.”
Where the System Is Breaking Down
The PBS works well for common conditions. 98% of hypertension drugs and 95% of diabetes meds are available as generics. But for rare diseases? The system stumbles. The HSDP has eight strict criteria. If a drug doesn’t meet all of them-even if it saves lives-it won’t be listed. A 2024 Senate inquiry found families waiting years for access to drugs that exist elsewhere. In response, the government relaxed two of the eight criteria in November 2025. That’s progress. But it’s still not enough.
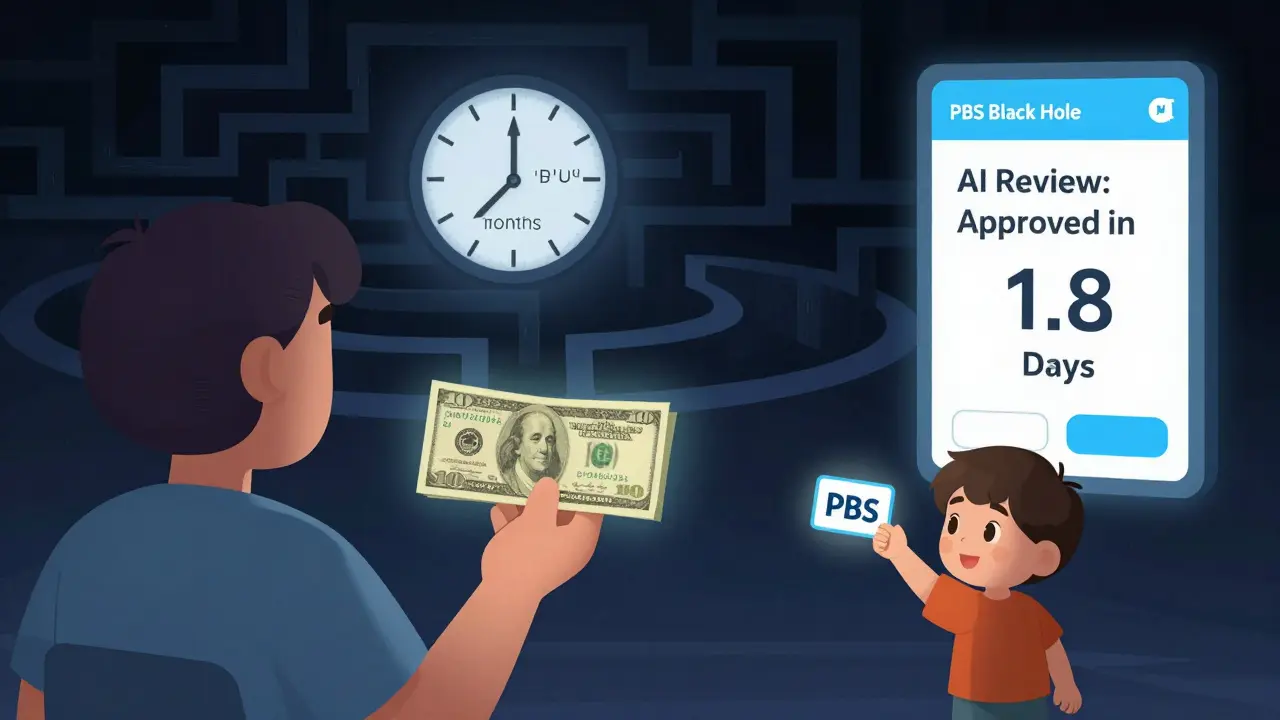
Another problem: delays after approval. The Therapeutic Goods Administration (TGA) approves a drug. Then it sits. On average, it takes 14.2 months for that drug to get listed on the PBS. That’s the “PBS black hole.” During that time, patients pay full price. In some cases, that’s over $10,000 a year. The government doesn’t track this gap closely. But the University of Melbourne’s 2025 study says it’s costing Australians $1.2 billion annually in unnecessary out-of-pocket costs.
The Future: Cheaper, Faster, Digital
The PBS is changing. The $25 co-payment in 2026 is just the start. The government is investing $1.2 billion in new listings for 2025-26, including drugs for prostate cancer and endometriosis. That’s 150,000 more Australians getting access. But the bigger shift is digital. The PBS app has been downloaded over 1.2 million times. Online authority requests now take 1.8 days on average, down from 7.3 days for paper. The Department of Health is testing AI tools to flag inappropriate prescriptions-like prescribing two similar drugs at once or giving long-term opioids without review. The 2024 Auditor-General found $1.2 billion in questionable PBS spending. AI might help cut that.
By 2030, PBS spending is expected to hit $18.7 billion. That’s driven by aging Australians, new high-cost biologics, and expanded uses for existing drugs. Experts warn this isn’t sustainable. Dr. John Skerritt, former Deputy Secretary of Health, says PBS costs could hit 2.6% of GDP by 2045-up from 0.7% in 2005. That’s more than Australia spends on public schools. But Professor Andrew Wilson, a health policy expert, counters: “The PBS saves households $13 billion a year. Without it, people wouldn’t take their meds. Chronic disease would explode. Hospitals would overflow.”
The truth? The PBS is messy, slow, and imperfect. But it’s also the reason millions of Australians can afford their prescriptions. It’s not perfect, but it’s working better than most systems in the world. The challenge now isn’t whether to fix it. It’s how to fix it without leaving anyone behind.
What is the PBS safety net and how does it work?
The PBS safety net is a cap on how much you pay for prescription medicines in a calendar year. In 2025, general patients pay $31.60 per script until they’ve spent $1,571.70 out-of-pocket. After that, they pay only $7.70 per script for the rest of the year. Concession card holders pay $7.70 per script until they hit $307.50, then they pay nothing. This prevents people with multiple chronic conditions from being priced out of care.
Why are generic drugs cheaper in Australia than in the U.S.?
Australia uses government-negotiated pricing and reference pricing. The PBS sets a maximum subsidy based on the cheapest drug in a therapeutic group. Manufacturers must compete on price, not branding. In the U.S., drug prices are set by private insurers and pharmaceutical companies with little government oversight. As a result, generic drugs in Australia cost 30-40% less than in the U.S., according to OECD data.
Can I get PBS-subsidized medicine if I’m not an Australian citizen?
Yes-if you’re from one of the 11 countries with a reciprocal health care agreement with Australia: New Zealand, the UK, Ireland, Sweden, the Netherlands, Finland, Italy, Malta, Norway, Slovenia, and Belgium. You must have a valid Medicare card. Visitors from other countries generally can’t access PBS subsidies unless they’re covered by private insurance or paying out-of-pocket.
Why do some drugs take so long to get listed on the PBS?
The PBS approval process involves clinical review by the PBAC, cost-effectiveness analysis, and budget impact modeling. A drug must prove it’s not only effective but also affordable compared to existing treatments. The average time from global launch to PBS listing is 587 days, with delays often caused by incomplete data submissions or negotiations over price. The government is trying to speed this up with digital tools and faster review pathways for high-need drugs.
How do I know if my medicine is on the PBS?
Your pharmacist will know immediately when you present your Medicare card. You can also check the PBS website (www.pbs.gov.au), which is updated monthly with new listings. The Services Australia PBS app lets you search by medicine name or condition and shows whether it’s subsidized, restricted, or requires authority. If you’re unsure, call 1800 020 299-the helpline handles over 1.7 million calls a year.
For those who rely on the PBS, it’s more than a policy. It’s a promise: that no one in Australia should have to choose between medicine and rent. The system isn’t flawless, but it’s the reason millions can breathe easier-literally.


Australia's PBS is one of those systems that looks boring until you need it. I’ve seen friends in the US pay $800 for a month’s supply of insulin while my cousin here pays $7.70. It’s not perfect, but it’s the closest thing we’ve got to healthcare that actually works for regular people.
Don’t let them fool you. The PBS isn’t saving anyone-it’s just delaying the inevitable. The government controls prices so hard that manufacturers stop innovating. You think generics are cheap? Wait until the next breakthrough drug never makes it here because the bureaucrats can’t agree on a price.
My dad’s on 5 meds and he’s a self-funded retiree too. $31.60 doesn’t sound like much… until you do the math for 6 months. I’m so glad they’re lowering it to $25 next year. It’s a small thing, but it matters. People don’t talk enough about how much stress this takes off families.
That stat about 12.3% skipping doses? Yeah. That’s not a number-it’s my neighbor. She’s got diabetes, hypertension, and a thyroid thing. She cuts her pills in half. I’ve seen her. She’s not lazy. She’s just out of options. The PBS is a lifeline, but it’s fraying at the edges. We need to fix the lag between TGA approval and PBS listing. That 14-month gap? That’s a death sentence for some.
It’s funny how the US talks about ‘free market’ healthcare while Australians get real value. The PBS doesn’t just cut prices-it cuts the nonsense. No fancy ads. No middlemen jacking up costs. Just ‘here’s the drug, here’s the price, now go live.’ It’s not glamorous, but it’s honest. And honestly? I wish we had this.
The real question isn’t whether the PBS works-it’s whether we’re willing to fund it properly. It saves $13 billion a year for households, but the government treats it like a budget line item, not a public good. If we valued health as much as we value roads or schools, we’d be funding faster approvals, better digital systems, and more biosimilar access. It’s not about cost-it’s about priorities.
As someone who works in health policy, I’ve studied systems across 12 countries. The PBS is uniquely effective because it combines price control with transparency. The PBAC’s QALY model isn’t perfect, but it’s consistent. And the digital shift? That’s the quiet revolution. AI flagging duplicate scripts? That’s not just efficiency-it’s preventing harm. This isn’t socialism. It’s smart governance.
I read this whole thing and just felt… seen. My mom has rheumatoid arthritis. She waited 2 years for her biologic to be listed. We paid $9,000 out of pocket. When it finally got approved, she cried. Not because it was free-because she didn’t have to choose between her meds and heating the house. The PBS isn’t flawless, but it gave her back her life. That’s worth more than any spreadsheet.
Just wanted to say-thank you for writing this. It’s easy to take the PBS for granted until you’re the one holding the prescription and the calculator. I’m glad we’re finally fixing the delays. And lowering the co-payment? That’s not just policy. That’s dignity.
While the PBS system demonstrates commendable cost containment and accessibility, the structural latency between therapeutic approval and subsidy inclusion remains a critical policy gap requiring immediate recalibration. The $1.2 billion in avoidable out-of-pocket expenditures, as cited by the University of Melbourne, constitutes a preventable fiscal and humanitarian burden that undermines the system’s foundational equity principle.