Most people know that a medication can cause a reaction right after taking it-hives, itching, or a quick rush of nausea. But what if your body doesn’t react until days or even weeks later? That’s when things get dangerous. These are called delayed drug hypersensitivity reactions, and they’re not just annoying rashes. They can be life-threatening, often mistaken for the flu or a virus, and they catch even doctors off guard.
What Exactly Is a Delayed Drug Reaction?
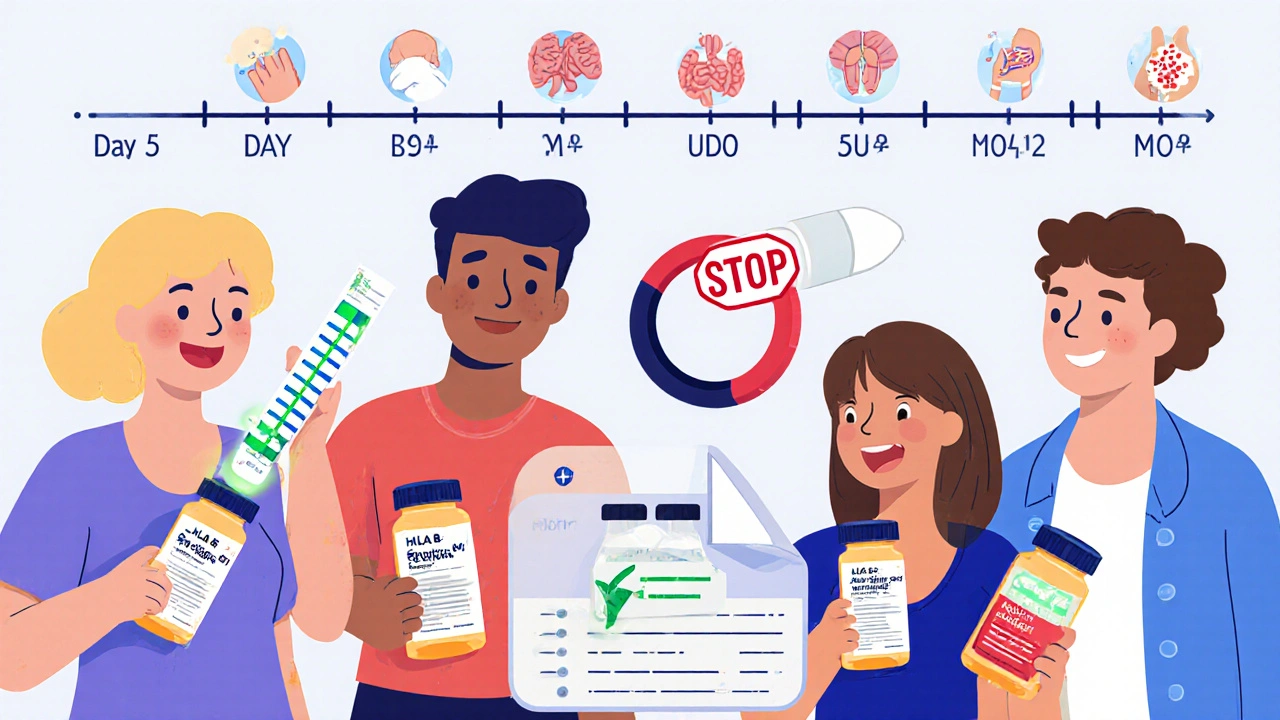
A delayed drug reaction is an immune system response that doesn’t show up until 5 days to 8 weeks after you start a medication. Unlike immediate allergies (like anaphylaxis from penicillin), these reactions are driven by T-cells, not antibodies. They’re part of what immunologists call Type IV hypersensitivity-the same mechanism behind poison ivy rashes or tuberculosis skin tests.
These reactions are far more common than most realize. About 80% of all drug hypersensitivity cases are delayed, according to the American Academy of Allergy, Asthma & Immunology. And they’re not rare: 1 to 5 people out of every 1,000 hospital admissions experience one. That’s tens of thousands of cases every year in the U.S. alone.
Common Types of Delayed Reactions
Not all delayed reactions look the same. They range from mild to deadly. Here are the main types:
- Maculopapular exanthema (MPE): This is the most common-about 80-90% of cases. It looks like a flat, red rash with small bumps. It usually shows up around day 8 after starting the drug and lasts 1 to 3 weeks after stopping it. People often think it’s a virus, especially if they had a cold or flu around the same time.
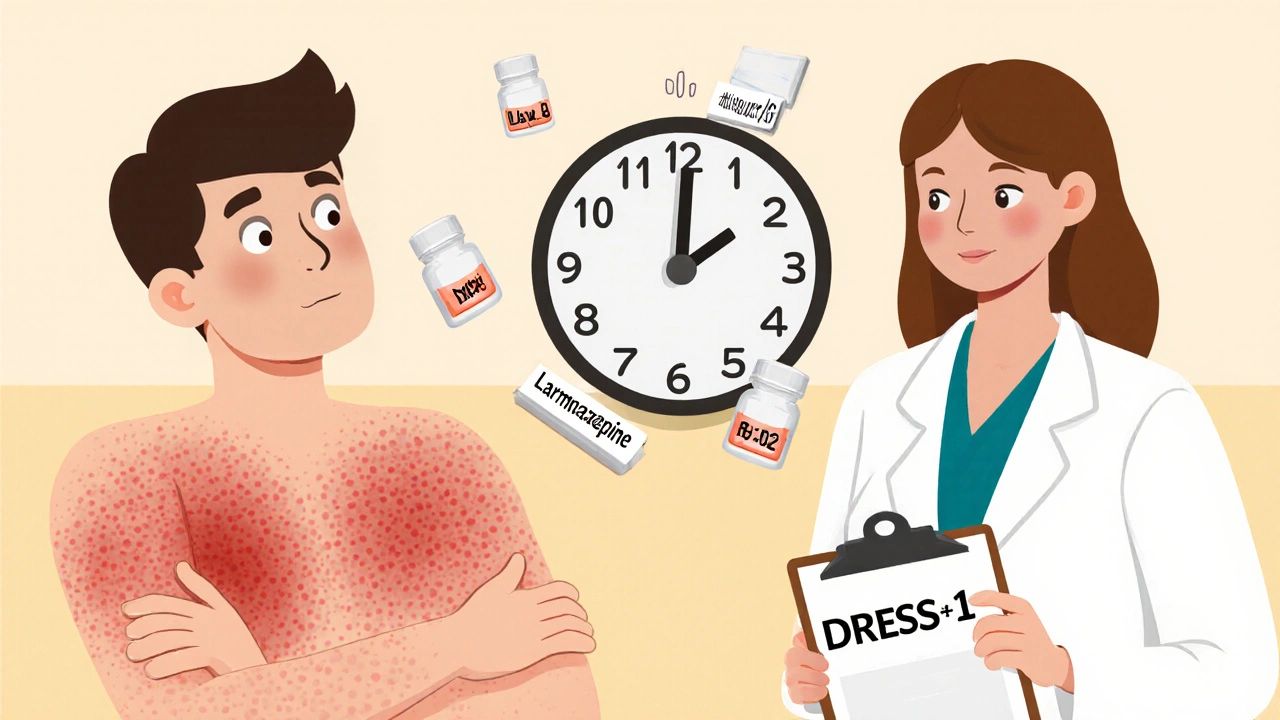
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): This one is serious. It involves fever over 38.5°C, swollen lymph nodes, high levels of eosinophils (a type of white blood cell), and organ damage-usually the liver, kidneys, or lungs. Onset is typically 2 to 8 weeks after starting the drug, with a median of 3 weeks. About 8% of people with DRESS die from complications like liver failure.
- Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN): These are medical emergencies. SJS causes skin detachment on less than 10% of the body; TEN affects over 30%. The skin blisters and peels off like a severe burn. Onset is usually 1 to 2 weeks after starting the drug. Mortality ranges from 5% to 10%, and if more than half the body is affected, it jumps to 30%.
- Acute Generalized Exanthematous Pustulosis (AGEP): This one comes on fast with hundreds of small, sterile pustules. It usually resolves within 15 days after stopping the drug, but it’s terrifying when it hits. The skin feels hot, tender, and looks like a bad acne breakout gone wild.
Which Drugs Cause These Reactions?
Some medications are far more likely to trigger delayed reactions than others. The biggest culprits:
- Anticonvulsants: Carbamazepine, phenytoin, lamotrigine, and oxcarbazepine. These are especially dangerous for people with certain genetic markers. For example, if you’re of Han Chinese descent and take carbamazepine, you have a 1,000+ times higher risk of developing Stevens-Johnson Syndrome if you carry the HLA-B*15:02 gene.
- Antibiotics: Penicillins, sulfa drugs like sulfamethoxazole, and cephalosporins. Even though people think of penicillin as an immediate allergy, many delayed reactions to these drugs show up 7 to 14 days after starting treatment.
- Allopurinol: Used for gout. If you’re of Thai, Korean, or other Southeast Asian descent and carry HLA-B*58:01, your risk of DRESS or SJS skyrockets. That’s why screening is now recommended before prescribing it in these populations.
- NSAIDs: Ibuprofen, naproxen, celecoxib. These can cause AGEP or MPE, especially in older adults.
Interestingly, the timing depends on the drug. Beta-lactam antibiotics usually trigger reactions within 2 weeks. But anticonvulsants? 92% of reactions happen after 2 weeks. That’s why doctors often miss the connection.
Why Do These Reactions Happen?
It’s not just “your body doesn’t like the drug.” There’s a precise biological reason. Three main theories explain how drugs trigger T-cells:
- The p-i concept: The drug binds directly to immune receptors (like HLA or T-cell receptors) without needing to change. This explains about 70-80% of cases. It’s like the drug is a fake key that accidentally fits the lock.
- The hapten theory: The drug attaches to a protein in your body, making it look foreign. Your immune system attacks it. This accounts for only 15-20% of cases.
- Altered peptide repertoire: The drug changes how your cells present proteins to T-cells, tricking them into attacking your own tissue.
Genetics play a huge role. Scientists have found over a dozen HLA gene variants linked to specific drug reactions. HLA-B*15:02 and carbamazepine. HLA-B*58:01 and allopurinol. HLA-A*31:01 and oxcarbazepine. These aren’t just correlations-they’re strong predictors. In some populations, testing for these genes before prescribing can prevent up to 80% of severe reactions.

How Are They Diagnosed?
There’s no single blood test. Diagnosis relies on three things:
- Timing: Did the rash or symptoms start 5 to 8 weeks after starting the drug?
- Clinical picture: Does it match RegiSCAR criteria? For DRESS, you need at least 3 of these: fever, swollen lymph nodes, eosinophilia, and organ involvement.
- Ruling out other causes: Viruses like EBV or HHV-6 can mimic DRESS. A doctor might run blood tests for those to be sure.
Drug rechallenge-taking the drug again to see if the reaction returns-is the gold standard. But it’s never done in suspected SJS, TEN, or DRESS. The risk of a second, worse reaction is too high. Instead, doctors use skin tests or lymphocyte transformation tests (LTT), which measure how T-cells react to the drug in a lab. LTT is 75-85% sensitive, but it’s not widely available.
What Happens If You Don’t Stop the Drug?
Delaying treatment is deadly. If you keep taking the drug after a delayed reaction starts, mortality jumps by 35%. In DRESS, continuing the drug can turn a mild liver enzyme rise into full-blown liver failure. In SJS/TEN, the skin keeps peeling, leading to sepsis, fluid loss, and organ shutdown.
One patient on Reddit described taking lamotrigine for 22 days before breaking out in a fever of 39.5°C. By day 28, her liver enzymes were over 1,200 U/L (normal is under 40). She spent 5 months recovering. She said: “I thought it was the flu. I didn’t connect it to the medicine until the ER doctor asked if I’d started anything new.”
How Are They Treated?
The first and most important step: stop the drug immediately. Even if you’re not sure it’s the cause, if the timing fits, stop it. Every hour counts.
Treatment depends on severity:
- Mild rashes (MPE): Usually just stop the drug and use antihistamines or topical steroids. They fade on their own.
- DRESS: High-dose corticosteroids (like prednisone at 0.5-1 mg/kg/day) are standard. Some hospitals use cyclosporine, especially if the kidneys are involved. Studies show it cuts recovery time by half compared to steroids alone.
- SJS/TEN: Treated like severe burns. You’re often moved to a burn unit. IV fluids, pain control, and infection prevention are critical. Steroids are controversial here-some doctors use them, others avoid them. There’s no clear consensus.
- AGEP: Stops quickly after drug withdrawal. Supportive care is usually enough.
Antibiotics are often given out of fear of infection, but they’re rarely needed unless there’s clear evidence of bacterial infection. In fact, continuing antibiotics in cases triggered by beta-lactams can make things worse-28% of patients who kept taking them developed more complications.
Long-Term Effects and Recovery
Recovery isn’t always quick. Even after the rash clears, problems linger:
- 35% of SJS/TEN survivors develop chronic eye problems-dryness, scarring, even blindness.
- 22% of DRESS patients develop autoimmune diseases like thyroiditis or lupus within two years.
- Hyperpigmentation (dark patches) can last 6 months or longer after AGEP or MPE.
- Many patients develop anxiety about all medications. One person on Inspire.com wrote: “I now refuse every new prescription. I’m terrified of another reaction.”
Recovery from DRESS can take 3 to 6 months. Liver enzymes might normalize in weeks, but fatigue, joint pain, and brain fog can last for months. Work productivity drops by 23% on average for 6 months after a DRESS episode.
What’s New in Prevention?
There’s hope on the horizon. In Taiwan, mandatory HLA-B*58:01 testing before prescribing allopurinol cut DRESS cases by 80%. Similar programs in Hong Kong and Thailand are showing the same results.
New tools are emerging:
- TCRβ sequencing can detect T-cells trained to react to carbamazepine with 92% accuracy.
- Serum CXCL10 levels above 150 pg/mL predict severe DRESS with 87% accuracy.
- AI systems are being trained to flag high-risk drug-HLA combinations in electronic health records before prescriptions are written.
But here’s the hard truth: current genetic tests only explain 40-60% of reaction risk. That means even if you test negative, you’re not safe. We still can’t predict all cases.
What Should You Do?
If you’ve started a new medication and develop a rash, fever, swollen glands, or unexplained fatigue after 5 days-don’t ignore it. Call your doctor. Don’t wait. Bring your medication list. Say: “Could this be a delayed drug reaction?”
Keep a list of all medications you’ve ever taken, especially ones that caused reactions. If you’ve had DRESS, SJS, or TEN, wear a medical alert bracelet. Avoid all drugs in the same class. For example, if you had a reaction to carbamazepine, avoid phenytoin, oxcarbazepine, and lamotrigine.
And if you’re of Southeast Asian descent and your doctor wants to prescribe allopurinol or carbamazepine, ask: “Should I get tested for HLA-B*58:01 or HLA-B*15:02 first?” That simple question could save your life.
Can delayed drug reactions happen with over-the-counter meds?
Yes. While most severe reactions come from prescription drugs like anticonvulsants or antibiotics, over-the-counter NSAIDs like ibuprofen and naproxen can trigger delayed rashes, especially in older adults. AGEP and maculopapular rashes are the most common reactions to these drugs. Don’t assume OTC means safe.
How long after stopping the drug does the reaction last?
It depends on the type. Mild rashes (MPE) usually fade in 1 to 3 weeks after stopping. DRESS can take 3 to 6 months for full recovery, even after the rash is gone. SJS/TEN skin re-epithelializes in 7 to 21 days, but internal damage and long-term complications like vision loss can last years.
Are delayed drug reactions hereditary?
Not directly, but your genetic makeup plays a big role. Specific HLA gene variants-like HLA-B*15:02 or HLA-B*58:01-are inherited and dramatically increase your risk for certain reactions. If a close relative had a severe reaction to a drug, you may be at higher risk for the same one. Genetic testing can help identify those risks before prescribing.
Can I ever take the drug again after a delayed reaction?
Never with severe reactions like DRESS, SJS, TEN, or AGEP. The risk of a second, potentially fatal reaction is too high. For mild rashes like MPE, some doctors may cautiously rechallenge under supervision-but this is rare and only done in controlled settings. Most patients are advised to avoid the drug and all similar ones for life.
Why do some people get these reactions and others don’t?
It’s a mix of genetics, immune history, and timing. People with certain HLA genes are at higher risk. Older adults, those with weakened immune systems, and people with chronic viral infections (like HIV or EBV) are more vulnerable. Also, taking multiple drugs at once increases risk. It’s not random-it’s biological, but we still don’t know all the triggers.

So I took ibuprofen for a week last winter and woke up with this weird rash that looked like chickenpox but didn't itch. Thought it was some weird virus. Turns out it was AGEP. Never touch NSAIDs again. Doctors don't even ask about OTC meds like it's harmless. Big mistake.
I work in a rural clinic and see this all the time. Elderly patients on multiple meds, get a rash, say 'oh it's just dry skin'-then end up in the ER with liver failure. We need better patient education. Not everyone has Google or a PhD in immunology.
Just read this whole thing. Mind blown. 😳 I was on lamotrigine for 3 weeks and got a tiny rash. Dr said 'probably nothing' and told me to keep taking it. I stopped anyway. Thank god. Now I'm scared to take anything. I keep a spreadsheet of every pill I've ever swallowed. 📊
Oh so now the government wants us to get genetic tested before we can take a painkiller? Next they'll be DNA scanning our toothpaste. 🙄
This is one of the most important medical posts I've read in years. The level of detail, the clarity, the urgency-it’s rare to see something this well-researched and accessible. Thank you for sharing this. I'm sharing it with my entire family and my doctor's office. Knowledge like this saves lives.
My cousin had DRESS after allopurinol. Took six months to recover. She still gets fatigued if she overdoes it. And now she's got autoimmune thyroiditis. It's not just 'a bad rash'-it rewires your body. I didn't even know HLA genes were a thing until this. Now I'm getting tested before any new prescription. Better safe than sorry.
I used to think doctors were all-knowing. Then I got a rash from sulfa and they thought it was a virus for three weeks. By then my liver was screaming. I swear, if you feel weird after a med-trust your gut. Don't wait for a textbook symptom. Your body talks. You just gotta listen.
This is all a big pharma cover-up. They don't want you to know how dangerous their drugs are. They're poisoning us slowly. HLA testing? That's just a way to charge you more. They want you to pay for genetic scans so they can keep selling you poison pills. The CDC knows. The WHO knows. They're all in on it. 😡
My mom had Stevens-Johnson from a penicillin shot 20 years ago. She still has vision issues. She wears sunglasses indoors now. I never realized how much damage these reactions do long-term. I always thought allergies were just sneezing or hives. This changed how I think about medicine. Thanks for writing this.
USA always overcomplicating everything. In India we just take medicine and if u get rash then stop it. No need for DNA test. HLA this HLA that. We have 1.4 billion people and we dont have time for all this science. Medicine is medicine. If it makes u sick then dont take it. Simple.
While the clinical information presented is accurate and valuable, the assertion that '80% of all drug hypersensitivity cases are delayed' requires contextual qualification. The American Academy of Allergy, Asthma & Immunology cites this statistic in reference to cutaneous reactions specifically-not all drug hypersensitivities, which include anaphylaxis, serum sickness, and other systemic phenomena. Precision in terminology is critical in medical communication.
As a pharmacogenomics researcher in Mumbai, I can confirm the HLA-B*58:01 screening protocol in India reduced allopurinol-induced SJS by 78% in our cohort. The real issue isn't the science-it's implementation. Rural clinics don't have access to PCR machines. We need decentralized testing, not just academic papers. Policy needs to catch up with genomics.