Anticoagulant Bleeding Risk Calculator
Bleeding Risk Assessment
This tool helps determine your bleeding risk profile to identify which anticoagulant may be most appropriate for you. Based on the American Heart Association's 5-point scoring system.
Choosing a blood thinner isn’t just about stopping clots-it’s about balancing safety, convenience, and your daily life. For millions of Americans with atrial fibrillation or a history of blood clots, the choice often comes down to two options: Direct Oral Anticoagulants (DOACs) or warfarin. While both do the same job-preventing dangerous clots-they do it in very different ways, and their side effect profiles can make one far better than the other for your situation.
How DOACs and Warfarin Work Differently
Warfarin has been around since the 1950s. It works by blocking vitamin K, which your body needs to make clotting proteins. That means your diet matters-eating a big plate of spinach or kale can throw off your dose. You also need regular blood tests (INR checks) to make sure you’re in the safe zone. Too low, and you risk a stroke. Too high, and you could bleed internally.
DOACs like apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa), and edoxaban (Savaysa) work differently. Instead of messing with vitamin K, they directly block specific clotting factors-either factor Xa or thrombin. That means no more weekly blood draws. No more worrying if your salad was too green. Dosing is fixed, usually once or twice a day, and you don’t need to adjust it based on food or most other medications.
Bleeding Risks: The Biggest Difference
The biggest reason DOACs replaced warfarin for most people is bleeding. A 2023 study of nearly 18,500 patients found DOACs cut hospitalizations for major bleeding by 31% compared to warfarin. That’s not a small edge-it’s life-changing.
Here’s the breakdown by type of bleeding:
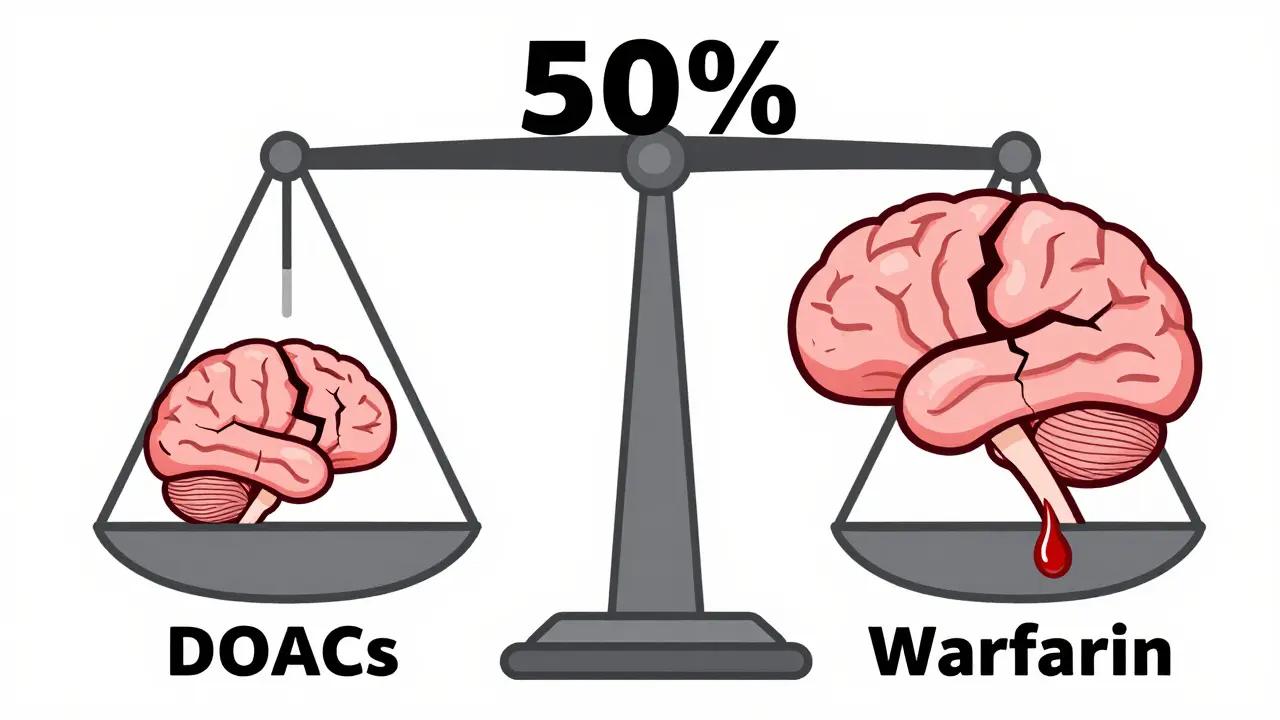
- Intracranial hemorrhage (brain bleed): DOACs reduce this risk by 50-60%. That’s huge. Brain bleeds are often deadly or disabling.
- Gastrointestinal bleeding: DOACs lower this risk overall, but not equally. Rivaroxaban carries a higher GI bleed risk than apixaban-1.35 times higher, according to a 2024 JACC study.
- Overall major bleeding: DOACs reduce it by about 30%. Apixaban leads the pack, with just 1.9 bleeding events per 100 patient-years, compared to 2.4 for warfarin and 2.8 for rivaroxaban.
That’s why experts now recommend apixaban as the go-to DOAC for older adults, especially those over 80. It’s the safest bet when bleeding risk is a top concern.
When Warfarin Still Wins
DOACs aren’t perfect for everyone. There are three key situations where warfarin remains the only choice:
- Mechanical heart valves: DOACs are FDA-approved to be avoided here. Studies show they increase the risk of clots forming on the valve, which can cause strokes or valve failure.
- Severe kidney disease: If your creatinine clearance is below 15-30 mL/min (depending on the DOAC), most DOACs aren’t safe. Warfarin doesn’t rely on the kidneys to clear out.
- Antiphospholipid syndrome: This autoimmune condition causes recurrent clots. A 2019 trial showed patients on DOACs had nearly three times the risk of new clots compared to those on warfarin. That’s why rheumatology guidelines still recommend warfarin here.
If you fall into one of these groups, warfarin isn’t outdated-it’s essential.
Cost and Convenience: The Real-World Trade-Off
Warfarin costs $4 to $10 a month. DOACs? Without insurance, $450 to $600. That’s a massive gap.
But here’s what most people don’t realize: the hidden costs of warfarin add up fast. Each INR test costs $30-$50. If you need one every two weeks, that’s $780 a year. Add in doctor visits, time off work, and the stress of unpredictable results, and warfarin starts looking expensive.
A 2024 study found DOACs become cost-effective after just 13 INR tests per year. Most warfarin patients need 20-30. Plus, 78% of DOAC users say their quality of life improved-mainly because they don’t have to plan meals around vitamin K or panic when their INR swings.
On Reddit and patient forums, warfarin users often say: “I had my INR checked every Monday. Sometimes it was fine. Sometimes it was dangerously high. I stopped eating spinach, then kale, then broccoli. I felt like I was on a diet I never asked for.”
What About Reversing the Blood Thinner?
What if you fall and hit your head? Or need emergency surgery? Can the drug be reversed?
Warfarin can be reversed with vitamin K or a concentrated clotting factor product called PCC. It takes hours to work, but it’s reliable.
DOACs have specific antidotes now, but only for some:
- Dabigatran: Reversed by idarucizumab (Praxbind), approved since 2015.
- Factor Xa inhibitors (apixaban, rivaroxaban, edoxaban): Reversed by andexanet alfa (Andexxa), approved in 2018.
- There’s no reversal agent for edoxaban in many hospitals.
And here’s the catch: these antidotes are expensive-$3,000 to $5,000 per dose-and not always available in rural or smaller hospitals. So while reversal is possible, it’s not always quick or easy.
Who Should Avoid DOACs?
Even if you’re not in one of the three special cases above, some people still shouldn’t take DOACs:
- People with very low body weight (under 60 kg or BMI under 18): DOACs may not be cleared properly, increasing bleeding risk.
- Those taking NSAIDs regularly: The FDA issued a warning in January 2024: combining DOACs with ibuprofen, naproxen, or aspirin raises GI bleeding risk by over 200% compared to warfarin with NSAIDs.
- Patients with poor kidney function: DOACs are cleared by the kidneys. If your CrCl drops below 30, you’ll need a lower dose-or switch to warfarin.
And don’t skip kidney checks. A 2022 audit found 18% of DOAC prescriptions were wrong because doctors didn’t recalculate kidney function after the patient’s weight dropped or after an illness.
Which DOAC Is Best?
Not all DOACs are the same. Here’s how they stack up for safety:
| Medication | Major Bleeding Rate (per 100 patient-years) | Best For |
|---|---|---|
| Apixaban (Eliquis) | 1.9 | Elderly, low body weight, history of falls, GI issues |
| Warfarin | 2.4 | Mechanical valves, antiphospholipid syndrome, severe kidney failure |
| Rivaroxaban (Xarelto) | 2.8 | Patients with good kidney function, no history of GI bleeding |
| Dabigatran (Pradaxa) | 2.2 | Patients who need reversal agent available |
| Edoxaban (Savaysa) | 2.1 | Patients needing once-daily dosing |
Apixaban consistently comes out on top. The American Heart Association now uses a 5-point scoring system to help pick the right drug: age over 75, kidney issues, past bleeding, taking aspirin or NSAIDs, and being female. If you score 3 or more, apixaban is the recommended choice.

Adherence Matters More Than You Think
DOACs have shorter half-lives. That means if you miss a dose, the drug leaves your system fast. Rivaroxaban’s half-life is just 7 hours. Skip one day, and your protection drops sharply.
A 2022 CVS Health analysis found 28% of warfarin users stopped taking it within a year. But only 18% of DOAC users quit. Why? Because warfarin is exhausting. Constant blood tests, dietary restrictions, and unpredictable results wear people down.
But DOACs aren’t foolproof. Many patients don’t realize they need to take them at the same time every day. One patient on PatientsLikeMe said: “I took my Eliquis at 8 a.m. one day, then 10 p.m. the next. I didn’t think it mattered. Turns out, it did.”
The Future: Cheaper DOACs and Smarter Dosing
Generic apixaban hits the market in 2026. Rivaroxaban will follow in 2027. That could cut DOAC costs by 80%-making them affordable even without insurance.
Researchers are also testing pharmacogenetic dosing. Some people metabolize apixaban slower because of their genes. The ELATES trial, launching in 2025, will test whether testing for these genes can make dosing safer and more precise.
And there’s new hope for reversal: two drugs in late-stage trials could reverse any blood thinner-DOAC or warfarin-with one shot. That could change emergency care forever.
Final Takeaway: It’s Not One-Size-Fits-All
DOACs are safer and easier for most people. But they’re not right for everyone. If you have a mechanical valve, severe kidney disease, or antiphospholipid syndrome, warfarin is still your best-and only-option.
For everyone else, apixaban is the gold standard. It’s the safest DOAC, with the lowest bleeding risk, and it works well even in older adults or those with other health issues.
Don’t let cost scare you off. Most insurance plans cover DOACs with a $30-$100 copay. And if you’re tired of weekly blood draws and worrying about your greens, the freedom DOACs give you is worth more than you think.
The right blood thinner isn’t the newest one. It’s the one that fits your life-and keeps you alive without making you miserable.


Let’s be real-DOACs aren’t just ‘better’; they’re a revolution in patient autonomy. I’ve seen grandparents go from living in fear of spinach salads to hiking, cooking, and traveling again. No more Monday INR panic. No more ‘did I eat kale yesterday?’ anxiety. Apixaban is the MVP here, especially for older adults. And yes, the cost is high upfront-but when you factor in the time off work, the lab fees, the stress-induced insomnia? It’s a net win. We’re not just treating clots; we’re restoring dignity.
Warfarin is still the gold standard for antiphospholipid syndrome. Anyone who says otherwise hasn’t read the 2019 trial data. Stop pushing DOACs like they’re magic pills.
Isn’t it poetic? We’ve traded centuries of bloodletting and herbal teas for a little pill you swallow while scrolling TikTok. We’ve outsourced our mortality to pharmacokinetics. Warfarin demanded mindfulness-daily rituals, dietary discipline, the hum of the INR machine like a metronome of life and death. DOACs? They’re the pharmaceutical equivalent of a self-driving car: convenient, impersonal, and terrifyingly easy to forget you’re not in control. And yet… we choose them anyway. Because freedom tastes better than fear-even if it’s just a placebo of control.
Hey, just wanted to say I’ve been on Eliquis for 3 years now-no issues. My mom was on warfarin for 8 years. She had three INR spikes that landed her in the ER. One time, she cried because she couldn’t eat her favorite spinach soup. I get why people love DOACs. It’s not just about the numbers-it’s about not feeling like a patient 24/7. Also, my pharmacist said generic apixaban’s coming in 2026. Thank god. That’ll be a game-changer for so many.
Okay so like… I’m not a doctor but I read a lot of med journals and I think the whole DOAC vs warfarin thing is being oversimplified. Like yeah apixaban is safer for bleeding but what about the fact that most people don’t even know they’re supposed to take it at the same time every day? I had this friend who took rivaroxaban at 8am one day and 11pm the next because she was ‘busy’ and then she had a minor GI bleed and the ER doc was like ‘did you take it regularly?’ and she was like ‘I thought it was like ibuprofen?’ and I was like oh my god we are literally giving people life-saving meds and treating them like they’re supposed to be pharmacists. Also the reversal agents? I went to a rural hospital last year and they didn’t have andexanet alfa. They had to fly in a helicopter with it. Like… is that really equitable healthcare? Also I think the FDA warning about NSAIDs and DOACs is underpublicized. Like my uncle takes naproxen for his arthritis and Eliquis and he didn’t even know it was a thing. He’s lucky he didn’t bleed out. We need better patient education. Like, not just pamphlets. Like actual conversations. Not just ‘take your pill’ but ‘here’s why your life depends on this’.
Apixaban isn’t ‘the best’-it’s the most profitable. Pharma pushed it because it’s easier to market than warfarin. The 31% bleeding reduction? Probably confounded by selection bias. Older, sicker patients are still on warfarin. Of course DOACs look better. Also, 18% of DOAC prescriptions are wrong because doctors don’t check kidney function? That’s not a flaw in the drug-that’s a flaw in the system. Stop pretending these are magic bullets.
Life’s too short for spinach anxiety. I switched to Eliquis after my third INR panic attack. I’m not a doctor, but I’m a dad who wants to see his kids grow up. DOACs gave me back my life. No more ‘is this salad safe?’ paranoia. I eat kale now. I sleep now. I travel now. That’s worth more than any pill price tag.
The data is clear: DOACs reduce intracranial hemorrhage by 50–60%. This is not a marginal gain. It’s a paradigm shift. The fact that clinicians still default to warfarin without evaluating renal function, weight, or NSAID use is negligent. This isn’t preference-it’s negligence masked as tradition. If you’re prescribing warfarin to an 82-year-old with a BMI of 17 and on naproxen, you’re not being cautious-you’re being reckless.
I’m a nurse who’s seen both sides. My patient, Mrs. Rivera, was on warfarin for 12 years. She missed work every Monday. She stopped seeing her grandkids because she was scared to fall. When she switched to apixaban, she started gardening again. She didn’t say much. But she brought me a jar of her homemade salsa one day. That’s the quiet victory here. Not the stats. Not the cost. The salsa.
Apixaban is the only ethical choice for elderly patients. Period. The fact that some doctors still push warfarin because ‘it’s cheaper’ is a moral failure. $4 a month? What’s the cost of a brain bleed? A stroke? A lifetime in a nursing home? You don’t save money by choosing warfarin-you just shift the burden to the system, to families, to ERs. And don’t even get me started on the ‘I don’t trust new drugs’ crowd. Warfarin was new once. So was penicillin. So was insulin. We don’t cling to leeches because ‘they worked for Galen.’