Entecavir isn’t just a pill you take once a day. It’s a lifeline for people living with chronic hepatitis B. But here’s the truth most people miss: taking entecavir doesn’t mean you’re cured. It means you’re managing a long-term condition - and that requires more than just swallowing a tablet. Without regular medical checkups, even the most disciplined patient risks serious, avoidable damage.
What Entecavir Actually Does
Entecavir is an antiviral drug approved by the FDA in 2005 for adults with chronic hepatitis B virus (HBV) infection. It works by blocking the virus from copying itself inside liver cells. That’s it. It doesn’t kill the virus. It doesn’t remove it from your body. It just slows it down. That’s why it’s called a suppressive therapy, not a cure.
People on entecavir often feel fine. No jaundice. No fatigue. No pain. That’s misleading. The virus can still be quietly replicating, slowly scarring your liver. Over time, that scarring turns into fibrosis, then cirrhosis. And cirrhosis can lead to liver cancer. The CDC estimates that 15-40% of untreated chronic HBV patients develop serious liver disease. Entecavir cuts that risk - but only if you’re monitored.
Why Your Doctor Needs to See You Every 6 Months
Most patients think, "I’m taking my pill. I’m fine. Why do I need to come back?" That’s the biggest mistake.
Here’s what your doctor checks during each visit:
- HBV DNA levels: This blood test tells you how much virus is still in your system. Even if you’re compliant, some people develop resistance. Entecavir resistance is rare - less than 1.2% after 5 years - but it happens. If your viral load starts creeping up, your treatment plan needs to change.
- Liver function tests (ALT, AST): These enzymes rise when your liver is inflamed. Normal levels mean your liver is calm. Rising levels mean it’s fighting back - even if you feel nothing.
- Alpha-fetoprotein (AFP): This is a tumor marker. A spike can signal early liver cancer. Catching it early means a 70-90% survival rate. Miss it, and survival drops below 20%.
- Ultrasound or FibroScan: Every 12-24 months, your doctor will check for liver scarring. Entecavir can reverse early fibrosis. But if you skip scans for three years, you might not realize your liver is already cirrhotic until it’s too late.
One patient I know - let’s call him Mark - took entecavir for six years without a single checkup. He felt great. Then he collapsed from internal bleeding. His liver had turned to stone. He needed a transplant. He’s alive today. But he lost five years of his life because he assumed the pill was enough.
What Happens If You Skip Checkups?
Skipping medical visits doesn’t mean you’re being rebellious. It usually means you’re overwhelmed, busy, or scared. But the consequences aren’t theoretical.
Studies from the Journal of Hepatology show that HBV patients who miss two or more checkups in a year are 3.5 times more likely to develop advanced liver disease. And 68% of those who end up in the ER with liver failure had not seen a specialist in over 18 months.
Entecavir works best when paired with surveillance. Think of it like this: your car’s oil change light doesn’t mean the engine is broken. It means it’s time to check. Same with entecavir. The pill keeps the engine running. The checkup tells you if anything’s wearing down.

Cost Isn’t the Real Barrier
Some people skip visits because they think it’s too expensive. But entecavir itself costs $1,200-$1,800 a year in the U.S. - and most insurance covers it. A single blood test? $50-$150. An ultrasound? $200-$400. That’s less than one month’s rent.
Compare that to the cost of liver cancer treatment: $100,000-$300,000. Or a transplant: $800,000. And that’s not counting lost wages, time off, or the emotional toll.
There are programs to help. The CDC’s Hepatitis B Foundation connects patients with free or low-cost testing. Many clinics offer sliding-scale fees. If you’re on Medicaid or Medicare, checkups are often fully covered. The barrier isn’t money. It’s awareness.
What to Bring to Your Appointment
Don’t walk in empty-handed. Bring this:
- Your pill bottle - even if it’s half empty. Your doctor needs to see your adherence pattern.
- A list of all other medications, supplements, or herbs. Some, like kava or high-dose vitamin A, can damage your liver.
- Notes on symptoms: dark urine? Itchy skin? Unexplained bruising? These aren’t "normal." They’re warning signs.
- Your last lab results - if you have them. It helps your doctor spot trends faster.
Also, ask: "Is my viral load undetectable?" If it’s not, you need to know why. And ask: "Should I be screened for liver cancer?" If you’re over 40, have cirrhosis, or have a family history of liver cancer - yes, you should be.
What Happens If Entecavir Stops Working?
Resistance is rare, but it happens. If your viral load rises, your doctor won’t panic. They’ll test for mutations. Then they’ll switch you to another antiviral - like tenofovir or tenofovir alafenamide. Both are highly effective, even if entecavir fails.
But here’s the catch: you won’t know it’s failing unless you get tested. You won’t feel it. You won’t see it. Your liver doesn’t scream. It whispers. And if you’re not listening, it stops talking altogether.
Staying on Track Long-Term
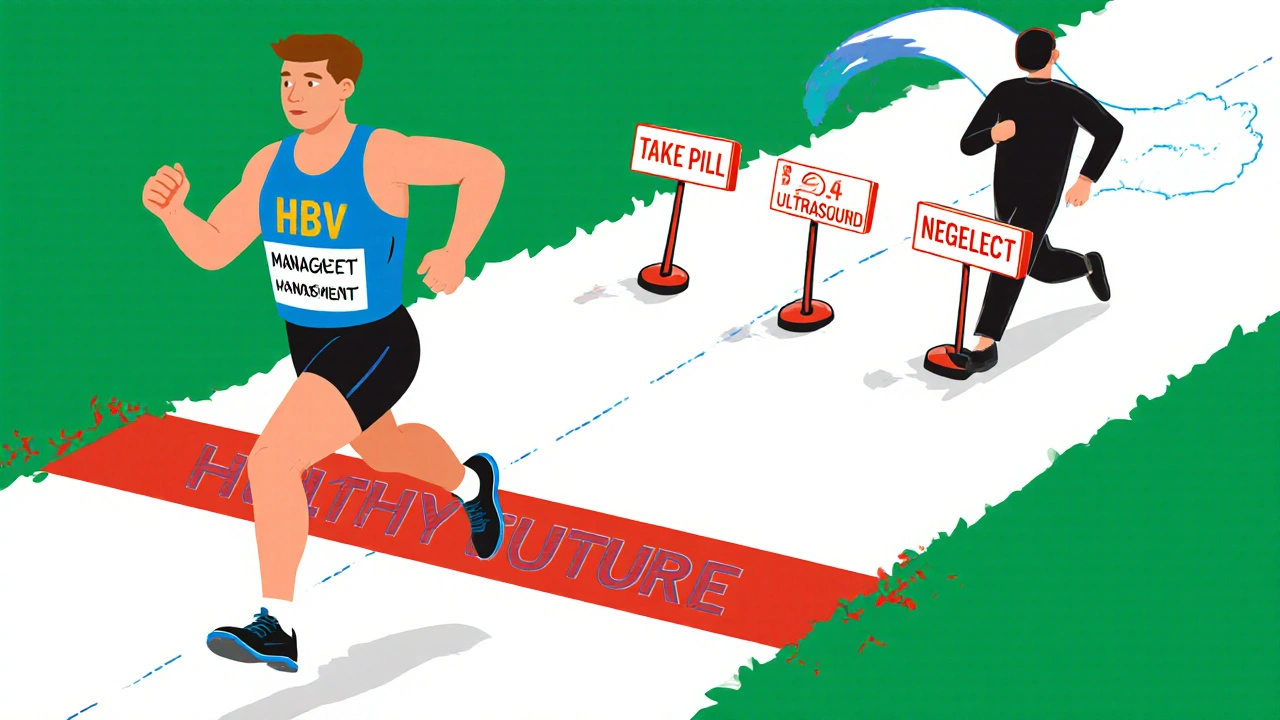
Managing hepatitis B isn’t a sprint. It’s a marathon with no finish line. You’ll need to stay on entecavir for years - possibly for life. That’s hard. But it’s easier when you build habits.
- Set phone reminders for your pills and your appointments.
- Keep a simple journal: date, pill taken, any symptoms.
- Find a support group. The Hepatitis B Foundation has online forums with thousands of people who’ve been where you are.
- Get vaccinated for hepatitis A. If you have HBV, getting hepatitis A can be deadly.
- Avoid alcohol. It doesn’t just hurt your liver - it makes entecavir less effective.
And never stop entecavir on your own. Stopping suddenly can cause a dangerous flare-up - a sudden, violent rebound of the virus. That can kill. Ever heard of acute liver failure from stopping antivirals? It happens. And it’s preventable.
Bottom Line: The Pill Is Only Half the Battle
Entecavir gives you control. But control requires accountability. You can’t manage a silent disease with silence. Regular checkups aren’t optional. They’re the second half of your treatment. They’re how you turn a lifelong condition into a manageable one.
Take your pill. Then show up for your appointment. That’s how you protect your liver. That’s how you protect your future.
Can entecavir cure hepatitis B?
No, entecavir cannot cure hepatitis B. It suppresses the virus to very low or undetectable levels, reducing liver damage and lowering the risk of cirrhosis and liver cancer. But the virus remains in the body. Most patients need to take it long-term, sometimes for life.
How often should I get blood tests while on entecavir?
Every 6 months. Your doctor will check your HBV DNA levels, liver enzymes (ALT, AST), and alpha-fetoprotein. If your condition is stable, some doctors may extend testing to once a year - but never skip more than 12 months.
What happens if I miss a dose of entecavir?
If you miss a dose, take it as soon as you remember - unless it’s almost time for your next dose. Don’t double up. Missing one dose occasionally won’t cause resistance, but frequent missed doses increase the risk. Consistency matters more than perfection.
Can I drink alcohol while taking entecavir?
No. Alcohol increases liver inflammation and can accelerate scarring - even if your viral load is undetectable. It also makes it harder for your liver to process the medication. Abstaining is the safest choice.
Is entecavir safe during pregnancy?
Entecavir is classified as Pregnancy Category C. It’s not routinely recommended during pregnancy, but if you’re on it and become pregnant, do not stop. Talk to your doctor immediately. Tenofovir is often preferred for pregnant women with HBV because it has more safety data. Never adjust your medication without medical guidance.
Do I still need liver cancer screening if my viral load is undetectable?
Yes. Even with undetectable virus, people with chronic HBV - especially those over 40, with cirrhosis, or with a family history of liver cancer - still need regular screening. The virus can cause damage before it’s fully suppressed. Ultrasound and AFP blood tests every 6 months are standard.


entecavir is not a cure?? duh. i took it for 3 yrs and still got cirrhosis. docs just wanna keep you on pills forever. my liver is toast and they said "at least you didnt die". smh.
Thank you for sharing this. I’m a nurse in Chicago and I see so many patients who think the pill is the whole story. You’re absolutely right - it’s like having a smoke detector but never checking the batteries. Regular labs aren’t a hassle, they’re a lifeline. And for those worried about cost - there are always options. Reach out. Ask. You’re not alone.
took entecavir 7 years. no checkups. felt fine. turned out my liver was 70% scarred. now on tenofovir. dont be me. get tested. its 50 bucks. save your life
Ugh. I hate when people act like this is some kind of moral failure. My cousin skipped checkups because she’s undocumented and terrified of the system. It’s not laziness - it’s systemic neglect. And now she’s in hospice. This isn’t about discipline. It’s about access.
Oh. My. GOD. You’re telling me… the virus doesn’t just VANISH?? Like… what? Did we all just assume it was a magic bullet?? I mean, I read the FDA label - it literally says "suppressive therapy" - but I thought that was just legalese. I’m 42, on entecavir since 2018, and I’ve been treating this like it’s a Netflix subscription - "I pay, I get to chill." Nope. Nope. Nope. I’m scheduling my ultrasound tomorrow. And I’m crying. Like, ugly, snorting tears. This is a wake-up call wrapped in a blood test.
You got this. Seriously. One step at a time. Set a phone alert for your next blood test. Write it on your mirror. Tell one friend. You’re not failing - you’re learning. And every time you show up for yourself, you’re rewriting the story. Your liver is fighting with you. Don’t let it fight alone.
Entecavir? LOL. I’ve got a friend who took it for 10 years and still got liver cancer. The whole system is a scam. Big Pharma doesn’t want you cured - they want you addicted to pills and checkups. 😔💸
It is imperative to underscore that the longitudinal monitoring of hepatitis B viral load, hepatic transaminases, and alpha-fetoprotein constitutes a standard-of-care intervention, as delineated by the American Association for the Study of Liver Diseases. Noncompliance with biannual surveillance protocols significantly elevates the risk of progression to hepatocellular carcinoma. The clinical imperative is unequivocal.
I used to think medicine was about fixing things. But hepatitis B… it’s not broken. It’s just there. Like a quiet roommate you can’t evict. Entecavir doesn’t kick it out - it just makes it stop throwing parties. The checkups? They’re the landlord knocking. "Hey, is everything okay in there?" And you have to answer. Even when you’re scared. Even when you’re tired. Because silence isn’t peace. It’s just waiting for the next storm.
My mate in Manchester had the same thing. Took the meds, skipped scans. Thought he was fine. Then he got dizzy, ended up in A&E with ascites. They said his liver was like a dried sponge. Now he’s on the transplant list. We’re all just one bad habit away from tragedy. Don’t be that guy. Get checked. Seriously.
But what if the checkups are just a money grab? What if the virus is harmless anyway? I mean, most people live with it and never even know. Maybe the whole "risk of cancer" thing is exaggerated to sell ultrasounds. I’ve read some papers that say HBV isn’t as deadly as they claim. Maybe we’re being manipulated.
Entecavir resistance is statistically negligible, yet you still fail to acknowledge that HBV is a preventable disease via vaccination. Why are we treating adults like children who need constant surveillance? The real failure is public health policy - not patient noncompliance. You’re blaming the victim while the CDC ignores primary prevention. Pathetic.
Look, I’m American. I don’t need some foreign virus telling me what to do. We got better things to worry about - like inflation and border security. This HBV stuff is just another liberal health scare. I take my pills. I’m fine. Let me live my life.
ok but like… 🥲 i just found out my dad has HBV and he skipped checkups for 8 years… i’m so scared. thank you for this post. i’m booking his appointment tomorrow. 🫶❤️