Brucellosis isn’t something most people think about unless they’ve been near livestock or eaten raw dairy. But if you’ve been exposed-maybe through unpasteurized cheese, handling newborn animals, or working on a farm-it can sneak up on you. Fever, sweats, joint pain, fatigue. It feels like the flu that won’t quit. And if it’s not treated right, it can stick around for months, even years.
Why Erythromycin Comes Up in Brucellosis Treatment
Brucellosis is caused by bacteria from the Brucella genus. The most common types in humans are Brucella melitensis, Brucella abortus, and Brucella suis. These bugs are tough. They hide inside cells, especially in the liver, spleen, and bone marrow. That’s why regular antibiotics often fail.
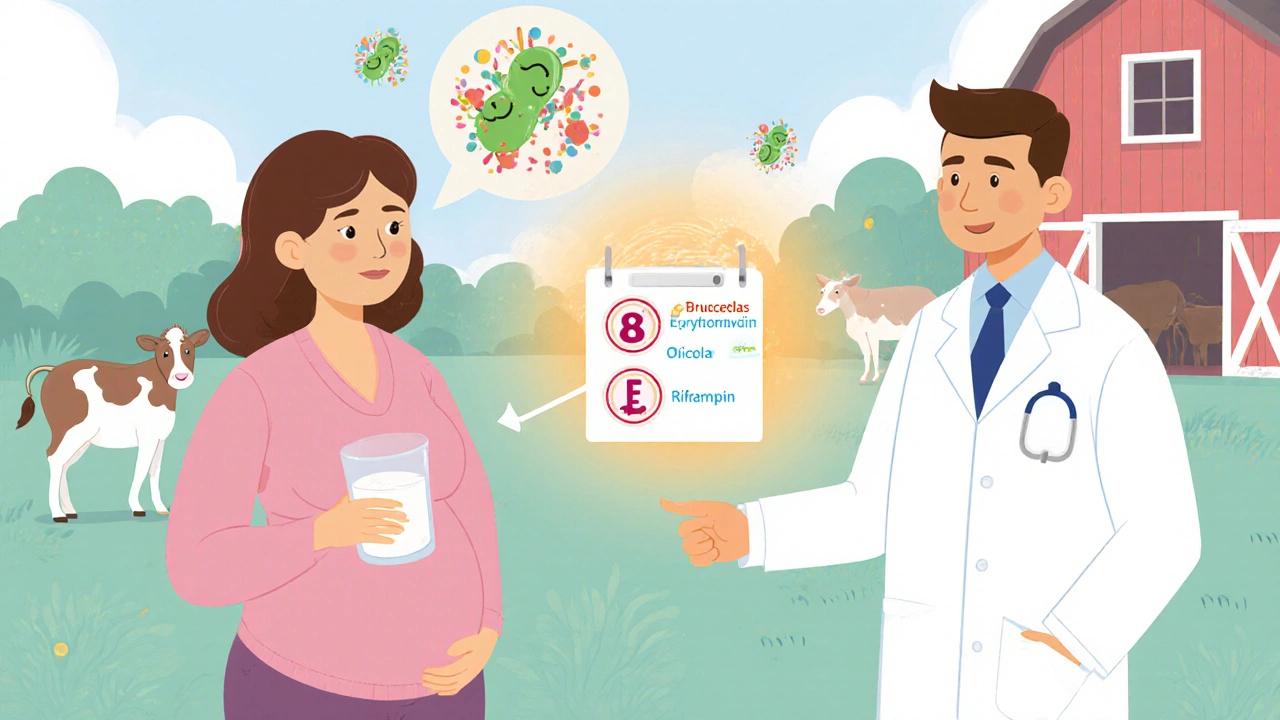
The standard first-line treatment is a combo of doxycycline and rifampin, taken for six weeks. But what if you’re pregnant? Allergic to tetracyclines? Or your doctor suspects a child has it? That’s where erythromycin steps in.
Erythromycin is a macrolide antibiotic. It doesn’t kill Brucella as fast as doxycycline, but it gets inside cells where the bacteria live. It’s also safe during pregnancy, which makes it one of the few options when you can’t use doxycycline. In kids under 8, doxycycline can stain developing teeth. Erythromycin doesn’t have that problem.
How Erythromycin Works Against Brucella
Erythromycin blocks protein production in bacteria. Without new proteins, the bacteria can’t grow or multiply. It’s bacteriostatic, meaning it stops them from spreading, giving your immune system time to clear the infection.
Studies show erythromycin penetrates macrophages-white blood cells that Brucella hides in-better than many other antibiotics. One 2020 review in the Journal of Antimicrobial Chemotherapy found erythromycin reached concentrations inside cells that were 3 to 5 times higher than in the bloodstream. That’s why it’s useful even when other drugs struggle.
But here’s the catch: erythromycin alone isn’t enough for long-term control. Brucellosis has a high relapse rate if treated with a single drug. That’s why it’s almost always paired with another antibiotic, usually rifampin.
Dosing Erythromycin for Brucellosis
Dosage depends on age, weight, and whether it’s being used alone or with another drug.
- Adults: 500 mg to 1 gram, taken 4 times a day, for 6 weeks
- Children: 30 to 50 mg per kg of body weight per day, split into 3 or 4 doses
- With rifampin: 600 mg daily, taken once a day
Always take erythromycin on an empty stomach-at least one hour before or two hours after meals. Food reduces how much your body absorbs. But if it upsets your stomach, taking it with a light snack is better than skipping the dose.
Some people think they can stop after feeling better. Don’t. Even if your fever drops in a week, the bacteria are still hiding. Stopping early is the #1 reason brucellosis comes back.
When Erythromycin Is the Best Choice
Not everyone needs erythromycin. But it’s the go-to in these situations:
- Pregnancy: Doxycycline is off-limits. Erythromycin + rifampin is the standard combo.
- Children under 8: Avoids tooth discoloration from tetracyclines.
- Allergy to doxycycline or tetracyclines: Erythromycin is a safe alternative.
- Chronic or relapsing cases: Sometimes used in longer regimens after first-line treatment fails.
In one case series from a veterinary hospital in Idaho, 12 pregnant women with confirmed brucellosis were treated with erythromycin and rifampin. All delivered healthy babies. None had relapses after six months of follow-up.

Side Effects and What to Watch For
Erythromycin is generally well-tolerated, but it’s not gentle. The most common issue? Upset stomach. Nausea, vomiting, cramps, diarrhea. Up to 30% of people report these, especially at higher doses.
It can also cause liver stress. Watch for yellowing skin, dark urine, or pain in the upper right abdomen. If you notice any of these, call your doctor right away.
Less common, but serious: heart rhythm changes. Erythromycin can prolong the QT interval, which may lead to irregular heartbeat. This risk goes up if you’re already on other QT-prolonging drugs-like some antidepressants, antifungals, or heart medications. Always tell your doctor what else you’re taking.
Some people get allergic reactions: rash, itching, swelling. Rarely, it causes a severe bowel infection called C. diff colitis. If you develop watery diarrhea that doesn’t go away after a few days, get tested.
How It Compares to Other Options
| Antibiotic | Best For | Duration | Pregnancy Safe? | Common Side Effects |
|---|---|---|---|---|
| Erythromycin | Pregnancy, children, tetracycline allergy | 6 weeks (with rifampin) | Yes | Stomach upset, liver stress, QT prolongation |
| Doxycycline + Rifampin | First-line for adults | 6 weeks | No | Sun sensitivity, stomach upset, liver enzyme changes |
| Trimethoprim-Sulfamethoxazole | Alternative for kids and non-pregnant adults | 6 weeks | Caution in 3rd trimester | Rash, low white blood cells, kidney issues |
| Fluoroquinolones (e.g., ciprofloxacin) | Adults with contraindications to other drugs | 6 weeks | Not recommended | Tendon damage, nerve issues, GI upset |
There’s no single best drug. It depends on who you are. For a 32-year-old man with no allergies, doxycycline + rifampin works best. For a 28-year-old pregnant woman? Erythromycin + rifampin is the clear choice.
What Happens If You Don’t Treat It
Left untreated, brucellosis doesn’t just fade away. It becomes chronic. Symptoms come and go. You might feel fine for weeks, then wake up with a fever again. Joints swell. Back pain becomes constant. Some people develop endocarditis-an infection of the heart valves. That’s life-threatening.
Neurological problems happen too: meningitis, encephalitis, nerve damage. In rare cases, it can cause infertility in men or miscarriage in women.
One study from Spain followed 187 untreated brucellosis patients for 10 years. Nearly half developed chronic symptoms. One in five had permanent joint damage. One in ten had heart complications.
Early treatment cuts relapse risk from 5-20% down to under 5%. That’s why starting the right antibiotics fast matters.

What to Do After Treatment
Even after finishing your antibiotics, you’re not done. Brucellosis can hide for months. Follow-up blood tests are critical.
Your doctor will likely order blood cultures and serology tests-like the standard agglutination test-at 1, 3, and 6 months after treatment ends. If titers stay high or rise again, it means the infection is still there.
Also, avoid raw milk, undercooked meat, and unpasteurized cheese. Re-exposure is the most common cause of recurrence. If you work with animals, wear gloves. Wash your hands. Don’t touch newborn lambs or calves without protection.
Frequently Asked Questions
Can erythromycin cure brucellosis by itself?
No. Erythromycin alone has a high relapse rate-up to 30%. It’s always used with another antibiotic, usually rifampin, to reduce the chance of the infection coming back. Combination therapy cuts relapse to under 5%.
Is erythromycin safe during pregnancy?
Yes. Erythromycin is classified as Category B by the FDA for pregnancy, meaning no evidence of harm in human studies. It’s the preferred antibiotic for pregnant women with brucellosis because doxycycline and fluoroquinolones are not safe. The combo of erythromycin and rifampin is standard in obstetric guidelines.
How long does it take for erythromycin to start working?
Fever and night sweats usually improve within 3 to 7 days. But that doesn’t mean the infection is gone. The bacteria are still hiding inside cells. You need the full 6-week course to kill them all. Stopping early is the main reason brucellosis returns.
Can you take erythromycin if you have liver disease?
Use with caution. Erythromycin is processed by the liver. If you have cirrhosis or severe liver impairment, your doctor may lower the dose or choose a different antibiotic. Liver enzymes should be checked before and during treatment.
Does erythromycin interact with other medications?
Yes. It can interact with statins (like simvastatin), some anti-anxiety drugs (like alprazolam), and medications that affect heart rhythm. It can also reduce the effectiveness of birth control pills. Always give your doctor a full list of everything you’re taking-prescription, over-the-counter, and supplements.
Final Thoughts
Erythromycin isn’t the flashy first choice for brucellosis-but it’s the quiet hero when you need it most. It’s the option that keeps pregnant women and young children safe. It’s the backup when allergies block other paths. It’s not perfect, but it’s reliable when used correctly.
Success doesn’t come from the drug alone. It comes from taking every pill, finishing the full course, watching for side effects, and getting follow-up tests. Brucellosis is a sneaky infection. It doesn’t care if you feel better. It waits. And if you don’t finish the job, it comes back.

Erythromycin’s real superpower isn’t killing Brucella-it’s sneaking into the cells where the bacteria hide like little ninjas. Most antibiotics just bounce off the surface, but this one goes deep. It’s not flashy, but it’s the quiet guardian when you’re pregnant or your kid’s under eight. We don’t talk enough about how medicine isn’t about the strongest drug, but the right one for the person.
It’s funny how we chase the newest antibiotics while ignoring the old ones that still work. Erythromycin’s been around since the 40s. It’s not glamorous, but it’s earned its place.
Still, I wish more doctors explained why combo therapy matters. People think if the fever’s gone, they’re fine. But Brucella’s not a sprint-it’s a marathon you can’t quit halfway.
bro erythromycin is literally just the backup plan lmao
doxycycline + rifampin is the OG combo, erythromycin is what you use when you’re allergic or preggo or your doc ran out of better options
also side effects?? bro i got diarrhea for 3 days straight on this stuff 😭
and dont even get me started on the QT prolongation-my aunt took this with her antidepressant and ended up in the ER. yall need to stop treating antibiotics like candy
Thank you for this detailed and clinically accurate overview. In Nigeria, where raw milk consumption is common and diagnostic access is limited, brucellosis remains underreported but devastating. Erythromycin’s role in pregnancy is particularly vital here, as many women present late and cannot afford multiple specialist visits.
However, adherence remains a challenge. Many patients stop medication when symptoms subside, not understanding the intracellular persistence of Brucella. Community health education must emphasize completion of the full 6-week course, even if they feel better after three days.
Also, we must acknowledge that in rural areas, access to rifampin is inconsistent. When erythromycin is used alone due to supply issues, relapse rates soar. This is not a pharmacological failure-it’s a systemic one.
okay but why is everyone acting like erythromycin is some kind of miracle drug??
it’s literally just the antibiotic you use when you’re too scared to use the real one
and the fact that it gives you diarrhea like you’re in a horror movie??
also why is this even a thing?? why are we still using 1950s antibiotics for modern infections??
someone’s making money off this and i’m not buying it
Did you know erythromycin was originally derived from soil bacteria in the Philippines? The same region where the CDC later found unregulated antibiotic runoff in rivers? Coincidence? I think not.
There’s a reason pharmaceutical companies push older drugs like this-they’re cheaper to produce, harder to patent, and less likely to be scrutinized. The FDA approved this combo decades ago without long-term reproductive studies.
And yet, we’re told it’s ‘safe’ for pregnancy? What about epigenetic effects? What about gut microbiome disruption in newborns? No one talks about that.
Just ask yourself: who benefits if you take this for six weeks? Not you.
OMG I JUST GOT BRUCELLOSIS FROM A PREGNANT FRIEND WHO TOOK ERYTHROMYCIN AND NOW I’M SCARED TO TOUCH A GOAT AGAIN 😭
like i get it, it’s ‘safe’ but what if it’s just… making the bacteria smarter??
also why does it taste like burnt plastic??
my doctor said ‘just finish the course’ but i’m pretty sure my liver is crying
someone please tell me i’m not the only one who thinks this is a scam
Interesting how the table compares antibiotics, but ignores cost and accessibility. In rural America, doxycycline costs $15 for a 6-week course. Erythromycin? $80. And that’s with insurance.
So when we say ‘erythromycin is the go-to for pregnant women,’ we’re assuming they can afford it. In reality, many choose to go untreated-or worse, self-medicate with leftover antibiotics.
Also, the QT prolongation risk is real, but rarely discussed outside cardiology circles. If you’re on a statin or antidepressant, you’re playing Russian roulette.
Medicine isn’t just about efficacy. It’s about equity. And right now, we’re failing that test.
There’s a deeper philosophical question here: if a drug doesn’t kill the pathogen outright, but only slows it down-allowing the immune system to do the real work-is it really ‘treating’ the disease?
Erythromycin doesn’t cure brucellosis. It buys time. It’s a pause button, not an off switch.
This reflects a broader truth in medicine: we often confuse intervention with healing. The body heals. Drugs just create the conditions.
Perhaps we should spend less time chasing new antibiotics and more time strengthening immune resilience through nutrition, sleep, and stress reduction.
Brucella doesn’t just infect the body. It infects the system. And we’re still treating symptoms, not causes.
My uncle was a vet in Montana. He treated 17 cases of brucellosis in farmers over 10 years. Every single one took erythromycin + rifampin because they were pregnant or had kids at home.
He always said, ‘It’s not about being the best drug. It’s about being the one that lets someone live their life.’
One woman gave birth to twins after finishing treatment. She sent him a photo of them holding a lamb. That’s why this matters.
Don’t reduce it to side effects or cost. For some people, this is the only thing standing between them and losing everything.
Y’all are overcomplicating this. Erythromycin isn’t perfect, but it’s the reason pregnant women aren’t losing babies to brucellosis. Period.
Yes, it causes stomach issues. So take it with a tiny bit of toast. Yes, it’s old. So what? Penicillin’s older and still saves lives.
And stop acting like the side effects are a conspiracy. They’re documented. Manage them. Don’t throw the baby out with the bathwater.
If you’re worried about relapse, get your follow-up tests. If you’re worried about cost, ask for generics. If you’re worried about your liver? Get labs done.
This isn’t magic. It’s medicine. And it works when you use it right.
THEY KNOW ERYTHROMYCIN IS WEAK SO THEY MAKE YOU TAKE IT WITH RIFAMPIN TO MAKE IT LOOK LIKE IT WORKS
THEY’RE HIDING THE RELAPSE RATES AND THE LIVER DAMAGE
AND WHY IS IT ONLY USED FOR PREGNANT WOMEN?? BECAUSE THEY’RE EASY TO CONTROL
THEY’RE USING YOU TO TEST NEW DRUGS AND THEY DON’T CARE IF YOU GET CHRONIC PAIN
LOOK AT THE TABLE-THEY DON’T EVEN LIST THE LONG-TERM NEUROLOGICAL EFFECTS
THIS IS A COVER-UP
WHO BENEFITS??
PHARMA
THEY’RE MAKING BILLIONS OFF YOUR FEAR
STOP TAKING IT
GO NATURAL
APPLE CIDER VINEGAR
AND DON’T TOUCH ANY ANIMALS EVER AGAIN
How quaint. You speak of erythromycin as if it were a noble remedy, but in truth, it is a relic of a bygone era-like using a quill pen to write a doctoral thesis. Modern medicine has moved on to targeted therapies, monoclonal antibodies, even CRISPR-based antimicrobials. Yet here we are, prescribing a macrolide from the 1950s because it’s ‘safe’ for pregnant women.
What a sad commentary on the stagnation of global health policy. We are not curing disease-we are managing mediocrity.
And yet, you praise its ‘reliability.’ Reliability is the refuge of the unimaginative.
Let’s be honest-erythromycin isn’t a treatment. It’s a compromise.
It’s what we give when we don’t have the guts to say, ‘We don’t have a good answer.’
We call it ‘safe’ for pregnancy, but we’ve never done a proper 20-year study on the children exposed to it in utero.
And the fact that we pair it with rifampin? That’s not science. That’s guesswork with a lab coat.
People think medicine is progress. It’s just a series of educated guesses we’ve been too afraid to admit are wrong.
And we keep doing this. Over and over.
Until one day, it isn’t just brucellosis that comes back.
It’s everything.
Just finished my 6 weeks. Fever’s gone. No relapse. No drama.
Took it with a banana. Didn’t die.
Worth it.
That’s the thing no one says out loud: the real hero isn’t the antibiotic. It’s the patient who showed up every day, even when they felt fine. Even when the pills tasted awful. Even when their doctor didn’t explain why it mattered.
That’s the quiet courage that actually cures brucellosis.
Not the drug. Not the combo. Not the guidelines.
The person who didn’t quit.