Imagine waking up soaked through, even though your room is cool. Your shirt sticks to your back. Your armpits are dark with sweat. You’ve been taking your antidepressant for weeks - your mood is better, but this sweating? It’s ruining your life. You’re not alone. About 1 in 10 people on antidepressants experience excessive sweating, a side effect so common it has a medical name: antidepressant-induced excessive sweating (ADIES). It’s not just uncomfortable - it’s embarrassing, exhausting, and sometimes enough to make people quit their medication altogether.
Why Do Antidepressants Make You Sweat So Much?
It’s not heat. It’s not exercise. It’s not anxiety - at least, not the kind you can control. Antidepressants like sertraline, paroxetine, venlafaxine, and even bupropion mess with your body’s internal thermostat. They boost serotonin, which is great for mood, but serotonin also talks directly to the hypothalamus - the part of your brain that controls sweating. When that signal gets mixed up, your body thinks it’s overheating… even when it’s not. This isn’t a rare glitch. Studies show 7% to 19% of people on SSRIs (the most common type of antidepressant) get this side effect. Paroxetine tops the list - nearly 1 in 5 users sweat excessively. Fluoxetine? Only about 7%. And then there’s citalopram - often a better choice for people who’ve had this problem before. Why? Because even though citalopram and escitalopram are almost the same drug, the way they’re structured in your body makes a real difference in sweating risk. Tricyclics and SNRIs like venlafaxine are also big culprits. Even bupropion, often praised for having fewer sexual side effects, can trigger sweating just as often as SSRIs. And here’s the kicker: this doesn’t always show up right away. Some people sweat normally for months, then suddenly start drenching their sheets at night. No warning. No pattern. Just sweat.Who’s Most Likely to Experience This?
It’s not random. Certain people are more vulnerable. Women report it more often than men, possibly due to hormonal differences in how the body regulates temperature. People who are already prone to sweating - even before starting medication - are more likely to see it get worse. Age matters too. Older adults may be more sensitive because their bodies process drugs slower, and their sweat glands become more reactive. The dose doesn’t always predict it. Some people get soaked on a low dose. Others take 100 mg of sertraline and barely notice. That’s why doctors can’t just say, “Take less.” Reducing your dose might make the sweating better - but it could also make your depression come back. And that’s not a trade-off most people are willing to make.What Medications Cause the Most Sweating?
Not all antidepressants are created equal when it comes to sweating. Here’s what the data shows:| Medication | Class | Estimated Sweating Risk | Notes |
|---|---|---|---|
| Paroxetine | SSRI | 19% | Highest risk - avoid if sweating is a concern |
| Sertraline | SSRI | 10-15% | Very common cause - many patient reports |
| Escitalopram | SSRI | 10% | Often replaced with citalopram to reduce sweating |
| Citalopram | SSRI | 7% | Lower risk than escitalopram - good alternative |
| Fluoxetine | SSRI | 7% | Lower risk, longer half-life |
| Venlafaxine | SNRI | 10-15% | Immediate-release worse than extended-release |
| Bupropion | NDRI | 8-12% | Similar risk to SSRIs despite different mechanism |
| Trazodone | SARI | 3-5% | Lowest risk among common antidepressants |
| Fluvoxamine | SSRI | 3% | Lowest sweating risk of all SSRIs |
Some people switch from escitalopram to citalopram - same dose, same class - and their sweating stops. Why? Because citalopram is a mix of two mirror-image molecules, and one of them (the S-form) is what makes escitalopram effective. The other molecule (R-form) might actually help balance out the sweating effect. It’s not fully understood, but it works for enough people that doctors now consider it a real strategy.
How to Cool Down: Practical, Real-World Strategies
You don’t have to suffer. There are things you can do right now - no prescription needed.- Wear moisture-wicking fabrics. Cotton holds sweat. Polyester, merino wool, or specialty blends like Coolmax pull moisture away and dry fast. Look for undershirts labeled “athletic” or “performance.” They’re cheap, and they make a huge difference.
- Use clinical-strength antiperspirant. Regular deodorant won’t cut it. Get one with 15-20% aluminum chloride. Apply it at night, on dry skin. Your armpits, chest, even the back of your neck - if you sweat there, treat it. It takes a few days to build up, but it’s one of the most effective non-drug fixes.
- Try a cooling vest. These aren’t sci-fi gadgets. They’re lightweight vests with gel packs or phase-change material that stays cool for hours. A 2022 pilot study showed a 60% reduction in sweating symptoms for people using them daily. You can buy them online for under $50.
- Keep your bedroom cold. Night sweats are the worst. Set your thermostat to 65°F or lower. Use a fan. Sleep on a cooling mattress pad. Wash your sheets more often - sweat builds up and makes the fabric feel sticky.
- Avoid triggers. Spicy food, caffeine, alcohol, and hot showers can all make sweating worse. You don’t have to give them up forever, but cutting back helps. Try switching from coffee to green tea - it’s lower in caffeine and has calming compounds.
When to Consider a Medication Switch
If cooling tricks aren’t enough, it’s time to talk to your doctor about switching. This isn’t giving up - it’s optimizing treatment. The best candidates for switching are:- People who’ve had bad sweating on sertraline or paroxetine
- Those who are stable on their current dose but can’t tolerate the side effect
- Anyone who’s tried lifestyle changes and still can’t sleep or function
- Citalopram instead of escitalopram
- Fluvoxamine - lowest sweating risk of all SSRIs
- Trazodone - often used for sleep, but also helps depression with minimal sweating
- Extended-release venlafaxine - if you need an SNRI, this version causes 23% less sweating than the regular kind
Don’t switch on your own. Stopping antidepressants suddenly can cause withdrawal symptoms - dizziness, brain zaps, nausea. Work with your doctor to taper slowly and introduce the new one gradually.
Medications That Can Help Reduce the Sweating
Sometimes, you need a second medication - not to treat depression, but to block the sweating.- Glycopyrrolate (1-2 mg daily): An anticholinergic that reduces sweat production. Side effects? Dry mouth, blurry vision. But for many, it’s worth it.
- Benztropine (0.5-1 mg daily): Often used for Parkinson’s, but it’s been shown to cut sweating by 75% in case studies.
- Terazosin (1-5 mg at night): A blood pressure drug that also blocks sweat signals. Works well for night sweats.
These aren’t first-line fixes. But if you’ve tried everything else and you’re still drenched, they can be game-changers. Your doctor can prescribe them off-label - meaning they’re not FDA-approved for sweating, but they’re proven to work.
When Sweating Is an Emergency
Not all sweating is ADIES. If you’re sweating and also have:- Fast heartbeat
- Muscle stiffness or tremors
- Confusion or high fever
- Shivering or seizures
…this could be serotonin syndrome. It’s rare, but deadly. It happens when too much serotonin builds up - often when you start a new drug or increase your dose. If you have these symptoms, go to the ER immediately. Don’t wait. Don’t call your doctor. Go.
What’s Coming Next
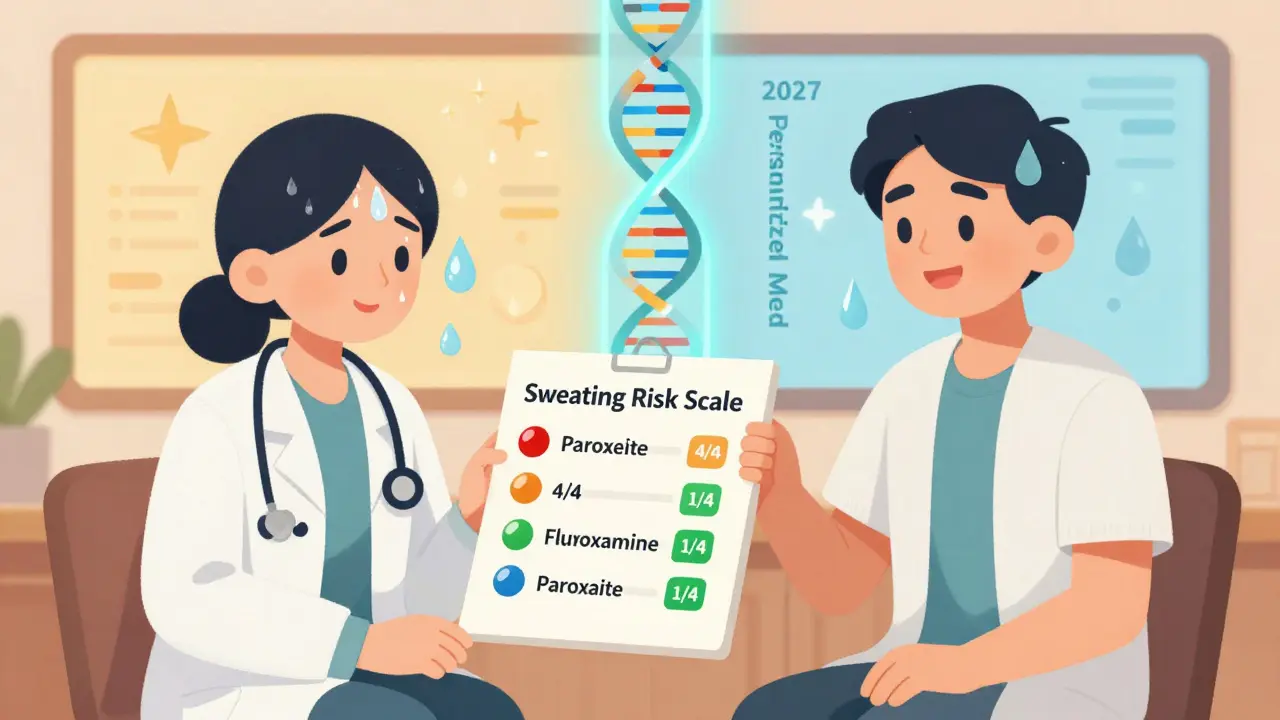
The future is getting better. In 2024, doctors started using a new tool called the Anticholinergic Risk Scale to predict which antidepressants are most likely to cause sweating. Paroxetine scores a 4 out of 4 - highest risk. Fluvoxamine? Just a 1. That’s helping doctors choose smarter. New drugs are in the pipeline. One called LS-2-1123, still in trials, caused only 3.2% sweating compared to 14.7% with escitalopram. That’s a massive improvement. And soon, genetic testing might tell you before you even start - “This drug will make you sweat. Try this one instead.” It’s not here yet, but it’s coming. By 2027, personalized medicine could cut ADIES rates by half.You’re Not Broken - You Just Need a Better Plan
Excessive sweating from antidepressants isn’t weakness. It’s biology. It’s not your fault. And it’s not permanent. Thousands of people have been where you are - stuck between feeling better mentally and feeling awful physically. The good news? You have options. You can tweak your meds. You can use cooling gear. You can try a different drug. You can add a tiny pill to calm the sweat. You don’t have to quit your antidepressant. You just need to work with your doctor to find the right combo for your body. Start with the simplest fix: switch to moisture-wicking shirts and use clinical antiperspirant at night. See if that helps. If not, ask your doctor about switching to citalopram or trazodone. Don’t let sweating steal your progress.Can antidepressants cause sweating even after years of use?
Yes. While many people experience sweating within the first few weeks of starting an antidepressant, it can also develop after months or even years of stable use. This is because the body’s response to serotonin changes over time, and some people develop increased sensitivity to the drug’s effects on sweat glands. If sweating starts suddenly after long-term use, don’t assume it’s unrelated - talk to your doctor.
Is excessive sweating from antidepressants dangerous?
The sweating itself isn’t dangerous, but it can lead to dehydration, sleep loss, and social anxiety - all of which can make depression worse. More importantly, sweating can be a sign of serotonin syndrome, a rare but life-threatening condition. If sweating comes with fever, rapid heartbeat, confusion, or muscle rigidity, seek emergency care immediately.
Will I sweat less if I reduce my antidepressant dose?
Sometimes, but not always. Studies show only about 40% of people see improvement in sweating after lowering their dose. For many, the sweating isn’t tied to how much they take - it’s about how their body reacts to the drug itself. Reducing your dose might help your mood return to worse levels, so this isn’t always a safe or effective solution.
Can I use over-the-counter sweat blockers?
Yes - but not the kind you use for normal body odor. Look for antiperspirants with 15-20% aluminum chloride, which are often labeled as “clinical strength” or “prescription strength.” Brands like Certain Dri or Drysol work well. Apply at night to dry skin, and wash off in the morning. It takes a few days to build up, but it’s one of the most effective non-prescription methods.
Are there antidepressants that don’t cause sweating at all?
No antidepressant is completely free of this side effect, but some have very low rates. Fluvoxamine causes sweating in only about 3% of users - the lowest among SSRIs. Trazodone is another low-risk option, especially if you’re also struggling with sleep. Newer drugs like vortioxetine and the upcoming LS-2-1123 also show promise for minimal sweating. Always ask your doctor about alternatives based on your personal risk profile.


Wow, this post is a lifeline. I’ve been sweating through my work shirts for 14 months on sertraline and thought I was just ‘bad at managing stress.’ Turns out it’s the meds. I switched to citalopram last month and my armpits are finally dry. Also started using Certain Dri at night-game changer. You’re not broken. You just need the right combo.
They’re hiding the real cause. Big Pharma doesn’t want you to know sweat is your body rejecting synthetic serotonin. The FDA knows. Doctors know. But they keep pushing SSRIs because the profit margin is insane. Try herbal adaptogens. Ashwagandha. Holy basil. Not pills. Real plants. They balance you without poisoning your glands.
People who blame their meds for sweating are just weak. I’ve been on 8 different antidepressants and never once sweated. You’re not ‘sensitive’-you’re lazy. Stop making excuses. Go to the gym. Drink water. Wear less clothing. Stop being a baby.
Okay but have y’all heard about the new LS-2-1123 drug? It’s like the holy grail. Only 3.2% sweating. I read the trial data. It’s not even in the U.S. yet because the FDA is corrupt. Big Pharma’s got patents on all the old crap. We’re being sold outdated tech while the real solutions sit in labs. Wake up. This isn’t medicine. It’s corporate control.
I’ve been on trazodone for 3 years. Zero sweat. Zero libido issues. Zero weight gain. I used to be on paroxetine and it felt like I was in a sauna 24/7. I cried in the shower every morning. Switching wasn’t easy-but it was worth it. You don’t have to suffer. Your brain deserves peace. Your body deserves comfort. Don’t settle for ‘it’s just a side effect.’ Fight for better.
Interesting how the table shows citalopram has lower sweating risk than escitalopram. But here’s the thing-most doctors don’t know this. I asked mine and she said ‘they’re the same.’ Nope. They’re not. The R-isomer in citalopram might be the secret buffer. I’ve seen it work. But if your doctor’s lazy, you’re stuck sweating. Knowledge is power. Print this post. Take it to your appointment.
They say ‘don’t quit your meds’ but what if your meds are making you hate yourself? I lost three jobs because I couldn’t show up without smelling like a gym bag. I tried the cooling vest. The antiperspirant. The dry clothes. Nothing worked. I went off sertraline cold turkey. Got brain zaps. Got depressed. But I didn’t sweat. And that’s the only thing I cared about. I’m not proud. But I’m alive. And I’m dry.
Let me guess-you’re all drinking green tea and wearing ‘moisture-wicking’ shirts like some wellness cult. Meanwhile, the real issue is electromagnetic pollution from 5G towers amplifying your body’s panic response. The sweat? It’s not serotonin. It’s your cells screaming from radio waves. The FDA won’t admit it. The WHO is paid off. Your ‘cooling vest’ won’t help. You need a Faraday suit. And a Geiger counter. Or are you too busy buying overpriced undershirts to see the truth?
Just wanted to say thank you for writing this. I’ve been too ashamed to talk about it. My husband thinks I’m ‘just hot-natured.’ I cried reading your section on night sweats. I started using the clinical antiperspirant last week. First night? Dry sheets. First time in 2 years. I’m not fixed. But I’m hopeful. And that’s enough for today. 💛