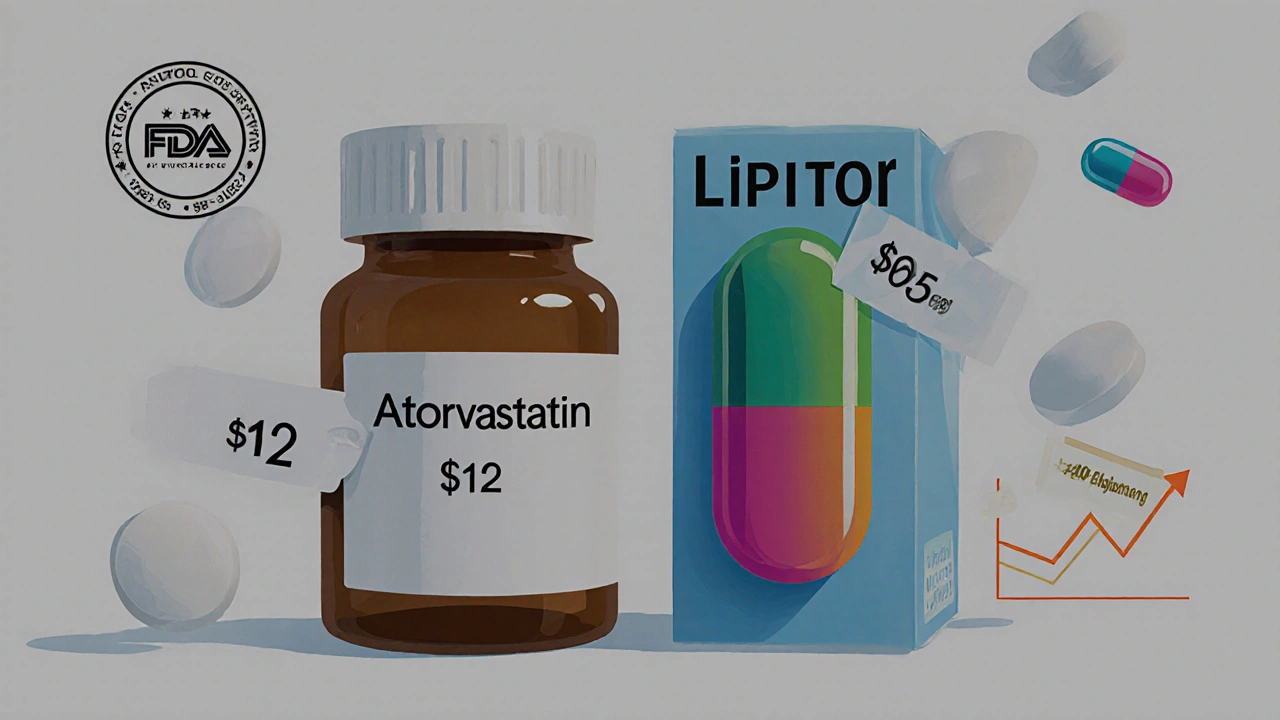
Let’s say you’re prescribed a medication for high blood pressure. At the pharmacy, you’re handed a small white pill in a plain bottle. The price? $12. A few weeks later, your neighbor gets the same medication - but it’s a colorful capsule in a branded box, and it costs $85. Same condition. Same doctor. Same pill, right? Not exactly. But here’s the truth: generic drugs are just as effective as their brand-name cousins. And they’ve been saving Americans billions every year.
What Exactly Makes a Drug "Generic"?
A generic drug isn’t a copycat. It’s not a cheaper version made with lower-quality ingredients. It’s an exact match - in every way that matters. The FDA requires that generic drugs contain the same active ingredient, in the same strength, same dosage form (pill, liquid, injection), and same route of administration (oral, topical, etc.) as the original brand-name drug.
For example, the generic version of Lipitor is atorvastatin. The generic version of Nexium is esomeprazole. The active ingredient is identical. That’s what your body reacts to. The rest? Color, shape, flavor, packaging - those are just cosmetic differences. U.S. trademark laws actually prevent generic drugs from looking exactly like the brand-name version. So if your pill changes color when you switch, don’t panic. That’s normal.
The FDA doesn’t just accept claims. Every generic drug must prove it’s bioequivalent to the brand-name drug. That means it delivers the same amount of active ingredient into your bloodstream at the same rate. The acceptable range? 80% to 125% of the brand’s absorption. For drugs with a narrow therapeutic index - like warfarin or levothyroxine - the range is even tighter: 90% to 111%. This isn’t a loophole. It’s a strict standard.
Why Are Generic Drugs So Much Cheaper?
Brand-name drugs cost a fortune because the company had to pay for everything: 10 to 15 years of research, clinical trials on thousands of patients, marketing campaigns, patent protection, and FDA application fees. That’s why a new drug can cost $2 billion to bring to market.
Generic manufacturers don’t have to do that. They don’t need to repeat expensive clinical trials. They just need to prove their version works the same way. That cuts development costs by over 90%. The savings get passed on. On average, generics cost 80% to 85% less than brand-name drugs. A 2022 University Hospitals analysis found the average savings per prescription was $313. That’s not a small discount - it’s life-changing for people on fixed incomes.
And the numbers back it up. In 2023, generics made up 90% of all prescriptions filled in the U.S. - but only 25% of total drug spending. Brand-name drugs, which make up just 10% of prescriptions, account for 75% of the money spent. That’s the power of generics.
Are Generic Drugs Safe? What Does the FDA Say?
Yes. They’re safe. The FDA holds generic drugs to the exact same standards as brand-name drugs for quality, purity, strength, and performance. Every facility that makes generics - whether it’s in the U.S., India, or China - is inspected by the FDA. The same rules apply. The same inspectors show up unannounced. The same quality controls are in place.
The FDA’s official stance is clear: "All drugs, including brand-name and generic, must work well and are safe." That’s not marketing talk. That’s policy. The agency monitors both types of drugs equally for adverse reactions. If a problem arises with a generic, the FDA investigates it the same way they would with a brand-name drug.
Pharmacists, doctors, and medical associations agree. The American Medical Association says doctors should prescribe generics when appropriate - to reduce costs without sacrificing outcomes. The FDA’s Orange Book, which lists all approved generic equivalents, currently includes over 10,000 generic products for more than 2,000 brand-name drugs. That’s not a small list. That’s the backbone of modern U.S. healthcare.

When Might You Still Want the Brand-Name Drug?
Most of the time, generics are the smart choice. But there are exceptions.
Some medications have a narrow therapeutic index - meaning even tiny changes in blood levels can cause problems. Warfarin (a blood thinner), levothyroxine (for thyroid disorders), and certain seizure meds like phenytoin fall into this category. Even though studies show no significant difference in outcomes between brand and generic versions, some doctors still prefer consistency. If you’ve been stable on a brand-name drug for years, switching might feel risky - even if science says it’s fine.
There are also rare cases where patients report feeling different after switching. On Reddit’s r/Pharmacy, one user said their mom’s seizures returned after switching from Lamictal to generic lamotrigine. Another said they felt foggy after switching from brand-name Adderall to generic amphetamine salts. These aren’t common - only about 14% of users in surveys reported issues - but they happen. Sometimes it’s the inactive ingredients (fillers, dyes, preservatives) that trigger sensitivities. Other times, it’s psychological. If you feel different, talk to your doctor. Don’t assume it’s all in your head.
For these cases, your doctor can write "dispense as written" on the prescription. That tells the pharmacy not to substitute. Most states require pharmacists to substitute generics unless that note is there. Forty-nine states have this rule. Only one doesn’t.
What About Complex Drugs? Inhalers, Creams, Injectables
Not all drugs are easy to copy. Inhalers, topical creams, and injectable biologics are much harder to replicate. Their effectiveness depends on how the drug is delivered - not just what’s inside. That’s why there are fewer generics for these types of medications.
For inhalers like Advair or Flovent, the device matters as much as the drug. The way the powder is dispersed, the particle size, the propellant - all affect how much gets into your lungs. Generic versions of these are called "authorized generics" or "biosimilars" and take years longer to develop. The FDA has identified 150 "complex generic" opportunities that could save billions if successfully made. But they’re technically challenging.
That’s why you might still see brand-name inhalers on the shelf - even if a generic exists. Sometimes, it’s because the generic hasn’t been approved yet. Other times, the manufacturer hasn’t bothered to make one because the market is too small. But that’s changing. With the FDA’s new GDUFA III rules, review times for generic applications are dropping. By 2027, they aim to cut approval time to 10 months. More generics are coming.

Real People, Real Savings
Most people don’t notice a difference. A 2022 Consumer Reports survey of over 1,200 people found 89% believed generics were just as effective. A Pharmacy Times survey showed 92% of patients preferred generics because of cost. One user on Reddit saved $400 a month switching from brand-name Advair to generic fluticasone/salmeterol - with zero loss in asthma control.
And it’s not just about monthly savings. For chronic conditions like diabetes, high cholesterol, or hypertension, you’re taking the medication every day for years. A $50 difference per month adds up to $600 a year. Over 10 years? $6,000. That’s a vacation. A new pair of glasses. A month’s rent. For many, it’s the difference between taking their meds or skipping doses.
From 2007 to 2016, generic drugs saved the U.S. healthcare system $1.67 trillion. Since 2017, they’ve saved an average of $253 billion per year. That’s not a number. That’s real people getting care they couldn’t otherwise afford.
What You Should Do Next
If you’re on a brand-name drug, ask your pharmacist: "Is there a generic version?" They can check instantly. If there is, ask your doctor if switching is safe for you. Most of the time, it is.
Keep a list of your medications - both brand and generic names. That way, if your prescription changes, you won’t be confused. GoodRx and other apps let you compare prices between brand and generic versions in real time. You might be paying more than you need to.
Don’t assume a higher price means better quality. Don’t assume a cheaper price means lower safety. The FDA doesn’t allow that. Generics are held to the same bar. The only real difference? The cost.
When you choose a generic, you’re not cutting corners. You’re choosing smart. You’re choosing to spend your money where it matters - on your health, not on a logo.
Are generic drugs as effective as brand-name drugs?
Yes. Generic drugs must meet the same FDA standards as brand-name drugs for active ingredients, strength, quality, purity, and performance. They are required to be bioequivalent, meaning they deliver the same amount of medication into your bloodstream at the same rate. Studies and real-world use confirm they work just as well for the vast majority of patients.
Why do generic drugs look different from brand-name drugs?
U.S. trademark laws prevent generic drugs from looking identical to brand-name versions. That’s why the color, shape, size, or packaging may be different. But the active ingredient - the part that treats your condition - is exactly the same. These differences are cosmetic and have no effect on how the drug works.
Can I trust generic drugs made in other countries?
Yes. The FDA inspects all manufacturing facilities - whether they’re in the U.S., India, China, or elsewhere - using the same strict standards. Over 80% of the active ingredients in U.S. generic drugs come from abroad, and every facility must pass FDA inspections before products are approved. The country of origin doesn’t determine safety - the FDA’s oversight does.
Why does my doctor sometimes prescribe the brand-name drug?
Doctors may prescribe brand-name drugs for medications with a narrow therapeutic index - like warfarin or levothyroxine - where even small changes in blood levels can affect outcomes. While studies show generics are safe for most patients, some doctors prefer consistency to avoid any potential risk. They can write "dispense as written" on the prescription to prevent substitution.
Are there any drugs that don’t have generic versions?
Yes. About 30% of brand-name drugs don’t yet have generic versions because they’re still under patent protection or are too complex to replicate (like certain inhalers, biologics, or topical creams). But over 450 brand-name drugs are expected to lose patent protection by 2028, which will bring many new generics to market in the coming years.
Will switching to a generic drug cause side effects?
For most people, no. But a small percentage report feeling different after switching - often due to inactive ingredients like dyes or fillers, or psychological factors. If you notice new symptoms after switching, talk to your doctor. It doesn’t mean the generic is unsafe - it just means your body might need time to adjust, or you may need to go back to the brand.

Generic pills are literally the same thing. Stop overthinking it. 💯
I switched my blood pressure med to generic last year and saved like $200/month. My doctor was skeptical but I told him to check the FDA data. No issues. My BP is stable, I feel fine, and I’m not broke. 🙌
This is such an important post! So many people are scared to switch because they think generics are "cheap" or "fake." But they’re literally the same medicine-just without the fancy packaging and marketing budget. I’m so glad we’re talking about this. 💙
India makes over 80% of the world’s generic drugs. We don’t cut corners. Our factories pass FDA inspections just like yours. The real issue? Pharma corporations don’t want you to know generics exist. They profit from fear. We’ve been doing this right for decades.
Let’s be real-90% of people who say "I feel different on generics" are just paranoid or lazy. The FDA doesn’t lie. If you’re having side effects, it’s either placebo or you’re not taking it right. Stop blaming the pill and start blaming your anxiety.
I used to be one of those people who refused generics because I thought brand-name meant better. Then my mom got diagnosed with diabetes and we couldn’t afford the $400/month for her insulin. We switched to generic metformin. She’s been on it for five years now. No complications. No issues. Just lower bills and better sleep. I just wish more people knew how safe and effective these are. It’s not a gamble-it’s science.
There’s a deeper philosophical question here: if a drug performs identically, but costs 1/5th the price, is it still the same object? Or has its essence been stripped away by capitalism? The pill doesn’t care about your brand loyalty. But you? You’ve been conditioned to equate price with worth. That’s not medicine-that’s mythology. And we’re all still paying for it.
Wait-so if generics are bioequivalent, why do some patients report different side effects? Is it possible that the inactive ingredients-like dyes, fillers, or preservatives-could trigger subtle immune or neurological responses in sensitive individuals? And if so, shouldn’t the FDA require more transparency around these additives? I’ve read studies where patients with histamine intolerance reacted to certain fillers in generics… it’s not placebo. It’s pharmacology. We need better labeling.
It is a matter of principle. One pays for quality. One pays for research. One pays for accountability. To choose a generic is to choose convenience over commitment. The brand-name manufacturer invested billions. The generic manufacturer invested nothing but a printing press. The difference is not in the pill-it is in the character of the consumer.
Oh wow, so you’re telling me the $85 pill isn’t magically better because it has a rainbow swirl? 🤦♀️ Thanks for the hot take, Big Pharma.
you think the fda is real? they get paid by big pharma. the generics are made in china and the pills are full of talc and asbestos. they want you to die slow so you keep buying. i saw a video where a guy opened a generic pill and it was just sugar and glitter. you believe this? you’re brainwashed. they control the meds, the news, even your dreams. wake up.
Why are Americans so obsessed with paying more for nothing? In Nigeria, we use generics for everything-malaria, HIV, hypertension. We don’t have luxury. We have survival. If it works, it works. Your system is broken. You pay for logos while your grandparents skip doses. Shame on you.