When you pick up a prescription, you might assume all generics are created equal. But that’s not true. Some generic drugs cost far more than others-even when they do the exact same thing. And when you compare buying two separate generics versus one combination pill, the difference in price can be staggering. The real savings aren’t always obvious. They’re hidden in the details: dosage forms, manufacturer competition, and whether your doctor prescribes separate pills or a single combo.
Why Some Generics Cost More Than Others
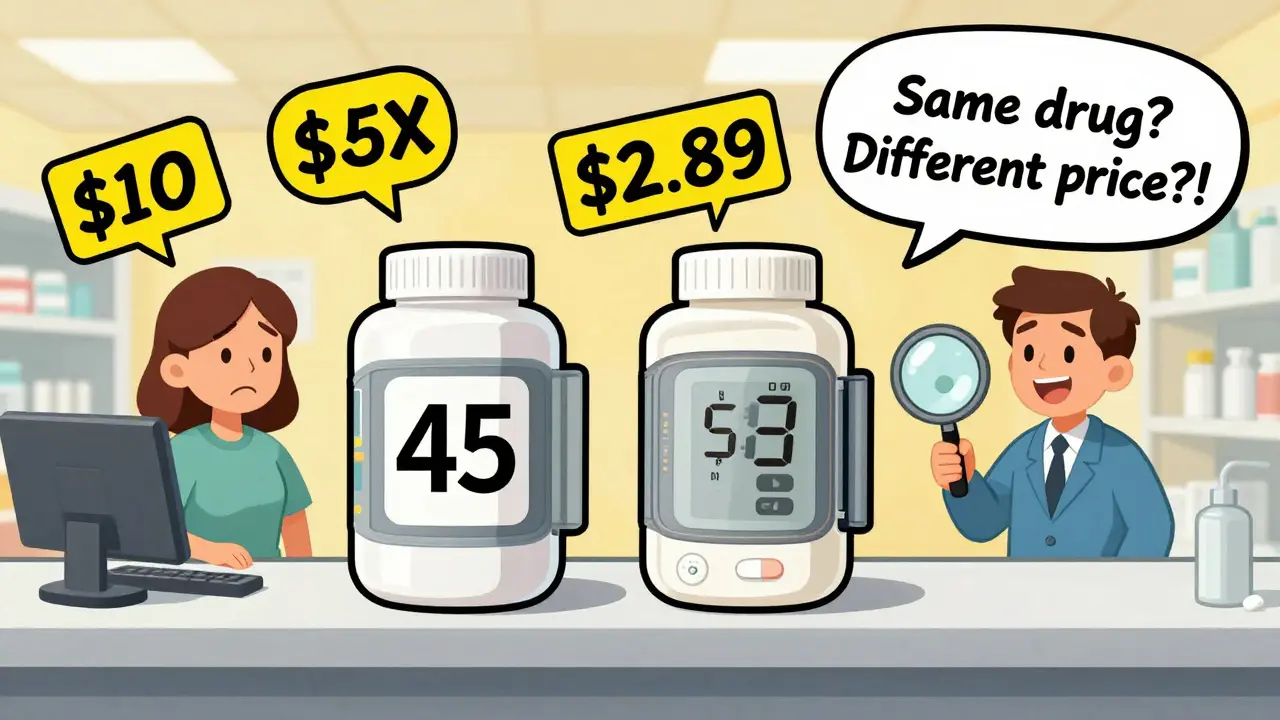
Not all generic drugs are cheap. A 2022 study of 1,000 top-selling generics in Colorado found that some were priced at 15.6 times more than their clinically equivalent alternatives. That’s not a typo. One generic version of a common blood pressure medication cost $45 per pill, while another version-identical in active ingredient, strength, and effect-cost just $2.89. The only difference? The manufacturer and the dosage form. The study found that 62% of these high-cost outliers could be replaced with a different strength or form of the same drug. For example, switching from a 10mg tablet to a 5mg tablet and splitting it in half saved 95% on average. Pharmacists can often make this swap without changing the treatment plan. But many prescribers don’t know about these options, and insurance plans don’t always encourage them. The reason? Some generic manufacturers hold onto high prices because they’re the only ones producing that exact formulation. When there’s only one or two makers, prices stay high. But when five or six companies start making the same drug, prices drop fast. The FDA found that with three competitors, prices fall about 20% within three years. With ten, they can drop 80% or more.Combination Drugs: One Pill, Big Savings
Combination drugs-like a pill that contains both an inhaled corticosteroid and a long-acting beta agonist (ICS/LABA)-were once only available as expensive brand-name products. Advair Diskus, for example, cost $334 per inhaler before generics hit the market. Then came Wixela Inhub, the first generic version. In just one year, the average cost dropped to $115. That’s a 65.6% cut in price per prescription. That’s not an outlier. Across the U.S., the introduction of generic ICS/LABA combinations saved $941 million in one year alone. Why? Because instead of buying two separate inhalers-one for the steroid, one for the bronchodilator-patients get both in one device. Fewer pills mean lower manufacturing, packaging, and distribution costs. And when multiple companies start making the same combo, prices plunge even further. The same pattern shows up in other areas. For blood pressure, diabetes, and HIV treatment, combination pills are now standard. A single pill with three active ingredients can cost less than buying each drug separately-even if all three are generics. In one 2023 analysis, a triple-combo HIV pill cost $12 per month, while the same three drugs bought individually totaled $47.Real Savings: What Patients Actually Pay
The savings aren’t just theoretical. A 2023 study of over 843 million prescription fills found that 11.8% of them had out-of-pocket savings when patients switched to a lower-cost generic or combination product. For uninsured patients, the savings were the biggest: 28.9% of their fills resulted in lower costs, with an average reduction of $6.08 per prescription. Even for people with insurance, the numbers add up. Medicare patients saved an average of $4.64 per prescription. Private insurance saved $3.69. Military insurance saved $5.05. These aren’t small amounts. Multiply that across millions of prescriptions, and you’re talking billions in savings every year. The Mark Cuban Cost Plus Drug Company, which sells generic drugs at near-wholesale prices, found that 28.4% of their prescriptions saved patients more than $10 per fill. That’s enough to cover a month’s worth of coffee, gas, or groceries for many people.
How to Spot High-Cost Generics
You don’t need a pharmacy degree to find better deals. Here’s how to check if your generic is overpriced:- Ask your pharmacist: “Is there a cheaper version of this drug in a different strength or form?”
- Check your insurance formulary. Look for alternative generics with an “A” rating in the FDA’s Orange Book-these are fully substitutable.
- Compare prices at different pharmacies. One CVS might charge $20 for a 30-day supply, while Walmart’s $4 list price is just $4.
- Ask your doctor if a combination pill is an option. For example, instead of metformin + sitagliptin as two pills, ask if Janumet (the combo) is right for you.
Barriers to Saving Money
It’s not all easy. Some high-cost generics stay expensive because of market manipulation. A few big companies control most of the generic supply. The top 10 manufacturers make up 40% of the U.S. generic market. That reduces competition and keeps prices high. Some insurance plans don’t automatically cover the cheapest option. They might favor a specific brand of generic because of rebates from manufacturers-even if it’s more expensive. That’s called “steering,” and it’s legal but not always in your best interest. Another issue: pharmacists can’t always substitute without a doctor’s OK. If your prescription says “Dispense as Written,” the pharmacist can’t switch you to a cheaper version-even if it’s identical. Always ask your doctor to write “Allow Substitution” or “Generic OK” on your prescription.
What You Can Do Today
You don’t have to wait for policy changes to save money. Here’s what to do now:- Review your last three prescriptions. Look up each drug on GoodRx or PharmacyChecker. Compare the lowest cash price to what you paid.
- If you’re on two or more separate generics for the same condition, ask if a combination pill exists.
- Ask your doctor to prescribe the lowest-cost generic with an FDA “A” rating.
- If your insurance denies a cheaper generic, file an appeal. Many plans will reverse the decision if you show the price difference.
- Use mail-order pharmacies or discount programs. Some save you 80% or more.
Why This Matters for Everyone
Generic drugs make up 90% of all prescriptions in the U.S. But they account for only 23% of total drug spending. That means they’re doing their job-cutting costs. But if we ignore the high-cost outliers, we miss half the opportunity. The U.S. spends over $1.2 trillion on prescription drugs each year. Experts project that better use of generics and combination products could save another $1.2 trillion over the next decade. That’s not just about insurance companies. It’s about patients who skip doses because they can’t afford their meds. It’s about families choosing between medicine and rent. The solution isn’t complicated. It’s simple: choose the cheapest effective option. Ask questions. Don’t assume your prescription is the cheapest one available. And if your doctor says “it’s the same,” ask: “Which same?”Are generic combination drugs as safe as brand-name ones?
Yes. The FDA requires generic combination drugs to meet the same safety, strength, quality, and performance standards as brand-name versions. They must contain the same active ingredients in the same amounts and work the same way in the body. The only differences allowed are in inactive ingredients like fillers or dyes, which don’t affect how the drug works.
Can I split a generic pill to save money?
Many generic pills can be safely split, especially if they’re scored (have a line down the middle). The FDA approves splitting for many drugs, including blood pressure and cholesterol meds. But not all pills are safe to split-especially extended-release or coated tablets. Always ask your pharmacist or doctor before splitting any pill.
Why does my insurance cover one generic but not another?
Insurance plans often choose generics based on rebates from manufacturers, not price. A more expensive generic might pay a bigger rebate to your pharmacy benefit manager (PBM), so the plan favors it-even if a cheaper version exists. You can appeal this decision by showing the price difference and asking for a formulary exception.
How do I know if a generic is FDA-approved?
Look for the “A” rating in the FDA’s Orange Book, which lists approved generic drugs and their therapeutic equivalence. If a generic has an “A” rating, it’s considered interchangeable with the brand-name drug. You can search the Orange Book online or ask your pharmacist to check it for you.
Do combination generics always cost less than buying two separate generics?
Usually, but not always. Combination pills are often cheaper because they reduce manufacturing and packaging costs. But in rare cases, a single generic might be priced unusually low-making two separate pills cheaper than the combo. Always compare the total cost of buying individual generics versus the combination before assuming one is better.

It’s wild how much variation there is in generic prices. I once paid $40 for a blood pressure pill only to find out the same thing at Walmart was $3. I felt like I’d been scammed. No one ever told me to ask about dosage alternatives. Pharmacists know this stuff. Doctors? Not so much.
Why do we assume the first prescription is the cheapest? We don’t do that with groceries. Why treat medicine differently?
Let’s be clear: the FDA’s therapeutic equivalence ratings are not suggestions-they’re regulatory mandates. If a generic has an ‘A’ rating, it is bioequivalent by design. The price disparities you’re observing stem from supply-chain monopolization, not pharmacological variance. The fact that 62% of high-cost outliers are replaceable with dosage adjustments speaks to systemic prescriber ignorance, not market failure.
Furthermore, the 80% price drop observed with ten competitors aligns perfectly with Cournot competition models. This isn’t anecdotal-it’s economic law. Stop treating pharmaceutical pricing like a lottery and start treating it like a regulated market.
OH MY GOSH, YES! I literally just switched my mom’s diabetes meds to a combo pill last month and she’s saving $80 a month-THAT’S A GROCERY SHOPPING SPREE! 🙌
And guess what? She’s taking her meds more consistently now because it’s ONE pill instead of three. No more morning pill organizer chaos. No more ‘did I take the metformin or was that the sitagliptin?’
Pharmacists are your secret weapon. Walk in, smile, and say ‘Is there a cheaper version?’ They’ll drop the truth on you like a gift. And if they say no? Ask for the Orange Book. They’ll blush.
Also-splitting pills? If it’s scored? YES. I split my 20mg lisinopril into two 10mg and saved $15. My heart thanks me. My wallet sings.
Doctors don’t always know this stuff. But YOU can. And when you do? You’re not just saving money-you’re reclaiming your health power.
PS: GoodRx is your new best friend. Bookmark it. Live on it. Love it.
I appreciate how detailed this is. It’s easy to feel overwhelmed by the system, but breaking it down into actionable steps-like checking the Orange Book or asking about dosage alternatives-makes it feel possible.
I’ve had friends who skip doses because of cost. This kind of information could literally change lives. Thank you for not just pointing out the problem, but giving people tools to fix it.
Back home in India, we’ve been doing this for years-splitting pills, buying generics from local pharmacies, switching brands based on price. It’s normal. Here, it feels like a secret you have to hunt for.
I remember my cousin in Delhi paying $0.20 for a month’s supply of metformin. Here? $40. It’s not the drug. It’s the system.
But I’m glad someone’s talking about it. Maybe more people will realize: medicine shouldn’t be a luxury.
My dad just got on Medicare and I helped him compare his prescriptions. We found he was paying $18 for a generic that was $2.50 on GoodRx. He was shocked. We called his doctor, switched it, and now he’s saving $400 a year.
It’s not hard. Just take 10 minutes. You don’t need a degree. Just curiosity and a little courage.
Combination pills are the real MVPs. I’ve got asthma and I used to pay $120 for two inhalers. Now I’m on Wixela and it’s $90. That’s not even the full story-my copay dropped from $50 to $15 because the combo was on a lower tier.
Also, splitting pills? I’ve been splitting my 40mg atorvastatin for years. No issues. My doctor was skeptical until I showed him the FDA guidelines. Now he recommends it to everyone.
Stop overpaying. You’re not being loyal-you’re being exploited.
My cousin in Texas got a $200 bill for a generic antibiotic. She called 12 pharmacies. The cheapest was a CVS in a strip mall that had it for $3.75. No insurance needed. She cried. I cried. We need to spread this word.
It’s not about being rich. It’s about being informed.
While the data presented may appear compelling, it is imperative to recognize that the U.S. pharmaceutical supply chain is subject to stringent regulatory oversight by the Food and Drug Administration. The notion that generic drugs are inconsistently priced due to market inefficiencies is an oversimplification that disregards the complex interplay of patent law, supply chain logistics, and contractual rebate structures between manufacturers and pharmacy benefit managers.
Moreover, the suggestion that patients should unilaterally alter dosage regimens without physician oversight constitutes a potential violation of standard-of-care protocols and may expose practitioners to liability.
It is not the fault of the system that some individuals fail to consult their healthcare providers prior to making therapeutic modifications.
Wait-so you’re saying I could’ve been saving $50 a month on my blood pressure med and I didn’t even know? I feel like I’ve been played.
But seriously, this is the kind of info that should be on every pharmacy receipt. Not just ‘Your copay is $20.’ But ‘You could’ve paid $5. Switch to this.’
Also, I just asked my doc about a combo pill for my cholesterol and diabetes. He said ‘Huh, good idea.’ I didn’t even have to push. Just asked.
Ask your pharmacist. Check GoodRx. Switch to combo if you can. Do it now.
It’s that simple.