Key Takeaways
- Secondary hyperparathyroidism (SHPT) often stems from chronic kidney disease and drives mineral imbalances.
- The excess parathyroid hormone (PTH) disrupts calcium and phosphate levels, directly affecting gut motility and absorption.
- Common GI complaints include nausea, constipation, diarrhea, and acid reflux.
- Treating SHPT with phosphate binders, vitamin D analogs, and dietary changes can relieve many digestive symptoms.
- Seek medical help if GI issues are persistent, severe, or accompanied by bone pain or abnormal lab results.
What Is Secondary Hyperparathyroidism?
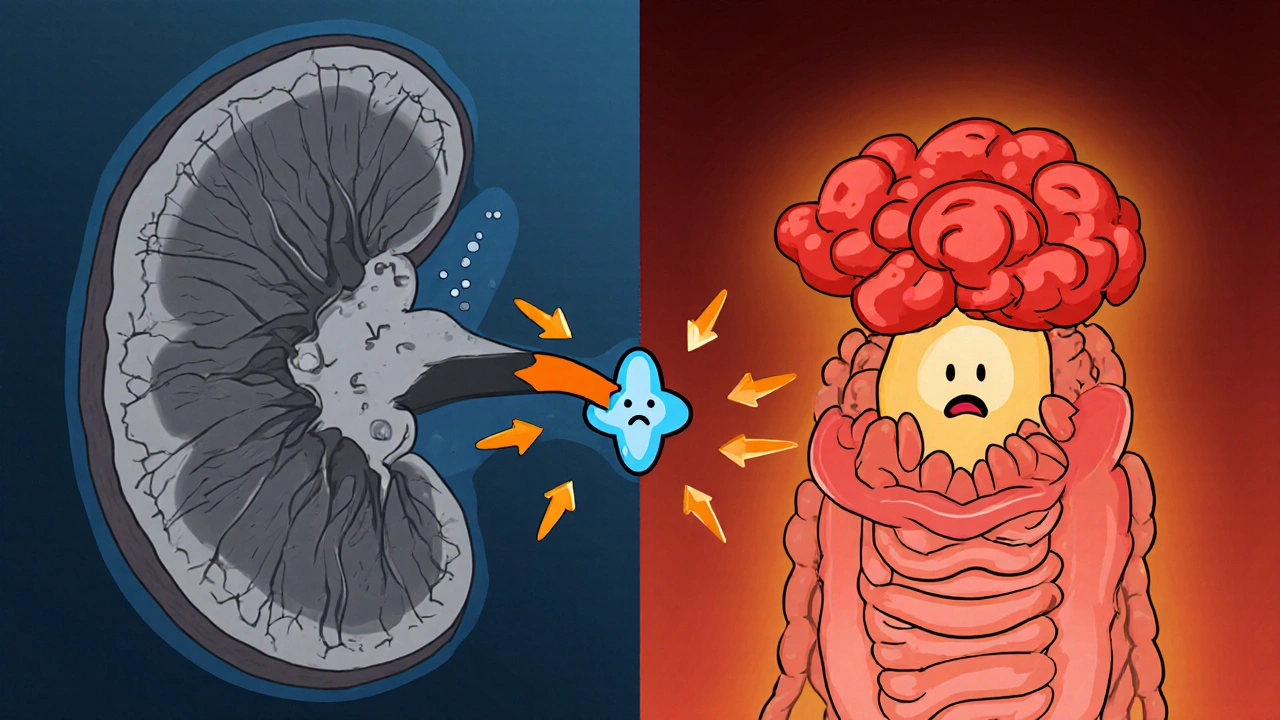
Secondary Hyperparathyroidism is a condition where the parathyroid glands overproduce parathyroid hormone in response to low blood calcium, usually because the kidneys can’t keep calcium balanced. It’s most common in people with chronic kidney disease (CKD). When kidneys fail to convert vitamin D to its active form and can’t excrete phosphate properly, calcium drops and PTH shoots up to compensate.
Why the Gut Gets Involved
The gut is the main highway for calcium and phosphate. When secondary hyperparathyroidism floods the bloodstream with PTH, it pulls calcium out of the bones and pushes phosphate into the bloodstream. This hormonal surge also changes how the intestinal lining absorbs nutrients.
Parathyroid Hormone is a regulator of calcium and phosphate metabolism that acts on bone, kidney, and intestinal cells. High PTH levels can:
- Increase renal phosphate reabsorption, worsening phosphate retention.
- Stimulate conversion of inactive vitamin D to its active form, but only if kidneys are functional.
- Alter smooth‑muscle tone in the gastrointestinal tract, leading to motility issues.
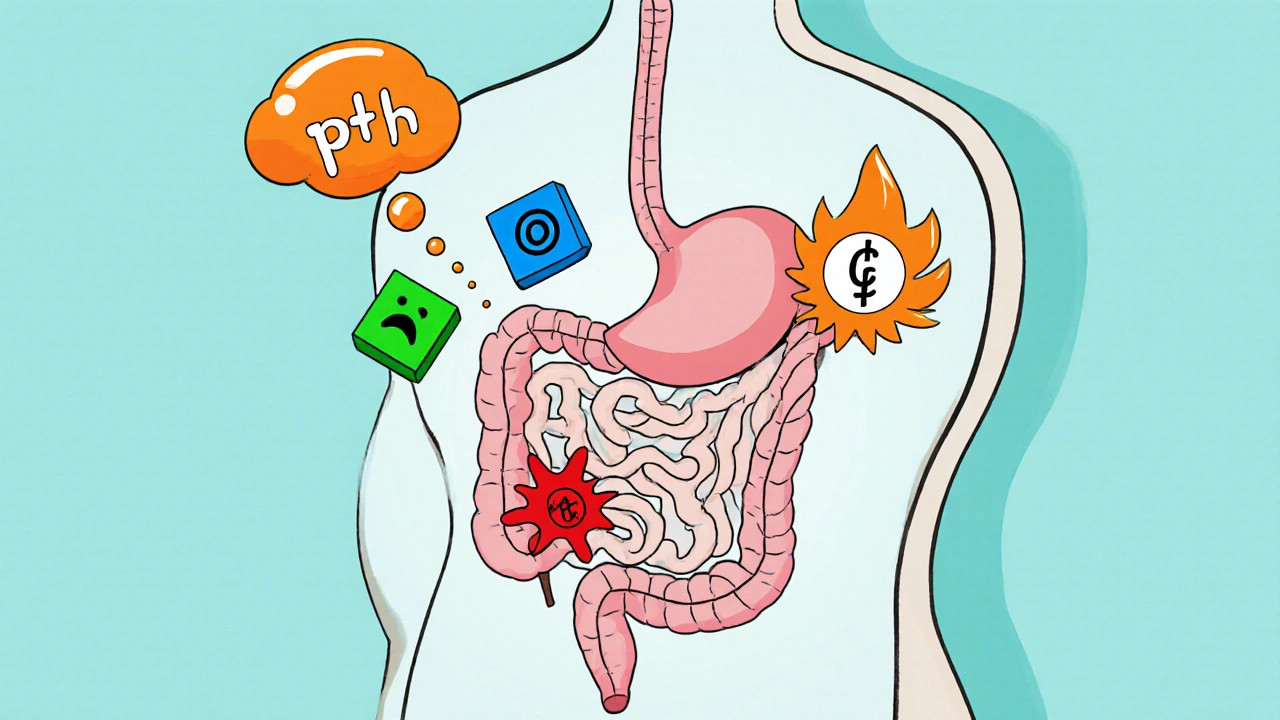
Key Players Behind the Symptoms
Several linked conditions drive the GI fallout:
- Chronic Kidney Disease reduces the kidney’s ability to activate vitamin D and excrete phosphate.
- Vitamin D Deficiency lowers calcium absorption in the gut, prompting more PTH release.
- Phosphate Retention raises serum phosphate, which together with low calcium triggers PTH secretion.
- Calcium Absorption is hampered by low active vitamin D and high phosphate, feeding the PTH loop.
- Bone Remodeling increases as PTH pulls calcium from bone, releasing cytokines that can affect gut nerves.
Typical Gastrointestinal Symptoms
People with SHPT often report a mix of digestive complaints. The table below matches common GI issues with the underlying hormonal or metabolic trigger.
| Symptom | Likely Cause in SHPT |
|---|---|
| Nausea & loss of appetite | Elevated PTH impacts gastric emptying and creates metabolic acidosis. |
| Constipation | Reduced smooth‑muscle motility from high calcium levels in the gut. |
| Diarrhea / loose stools | Phosphate overload and malabsorption of fats due to low vitamin D. |
| Acid reflux / heartburn | Altered lower esophageal sphincter tone from PTH‑induced calcium shifts. |
| Abdominal cramping | Electrolyte imbalances (calcium, magnesium) affecting nerve excitability. |
How the Hormone Messes With the Gut
The gut‑brain axis is sensitive to calcium flux. When PTH spikes, calcium moves out of the bloodstream into bone and intestine cells. This shift can:
- Disrupt the contractility of intestinal smooth muscle, slowing peristalsis and causing constipation.
- Increase secretion of gastric acid, leading to reflux and ulcer‑like discomfort.
- Change the composition of the gut microbiome; excess phosphate feeds harmful bacteria, which produce gas and cause bloating.
- Trigger inflammatory cytokines from bone turnover that travel via the bloodstream and irritate the intestinal lining.

Managing Both the Hormone and the Stomach
Effective treatment targets the root cause (the kidney‑related mineral imbalance) and the secondary gut symptoms.
- Phosphate Binders: Calcium‑based or non‑calcium binders lower serum phosphate, reducing PTH drive.
- Active Vitamin D Analogs (e.g., calcitriol): Boost intestinal calcium absorption, helping normalize blood calcium without over‑stimulating PTH.
- Dietary Adjustments: Limit high‑phosphate foods (processed meats, sodas), increase leafy greens for natural calcium, and ensure adequate magnesium.
- Probiotics: Support a balanced gut microbiome, which can lessen bloating and diarrhea.
- Fiber & Hydration: Helps counteract constipation caused by altered smooth‑muscle tone.
In some cases, doctors prescribe calcimimetic agents (e.g., cinacalcet) that make the parathyroid glands think calcium is higher than it is, lowering PTH production.
When to Seek Professional Help
If GI problems linger for more than a couple of weeks, are severe, or come with other red flags-such as bone pain, unexplained weight loss, or lab values showing calcium < 8.5 mg/dL or phosphate > 5.5 mg/dL-schedule an appointment. Early intervention can prevent long‑term bone disease and chronic digestive issues.
Frequently Asked Questions
Can secondary hyperparathyroidism cause weight loss?
Yes. Persistent nausea, reduced appetite, and malabsorption can lead to gradual weight loss if the underlying hormone imbalance isn’t corrected.
Is it safe to take over‑the‑counter antacids for reflux caused by SHPT?
Occasional antacids are usually fine, but they can add extra calcium or aluminum, which might worsen phosphate imbalance. Talk to your doctor before making them a regular habit.
Do I need to stop calcium‑rich foods?
Not completely. Your body still needs calcium, but you may need to balance intake with phosphate binders and monitor blood levels under medical supervision.
Can probiotics really help my stomach?
Probiotics can restore a healthier gut flora, which may reduce diarrhea and gas caused by phosphate‑driven bacterial overgrowth. Choose strains with Lactobacillus and Bifidobacterium for best results.
What lab tests should I ask for?
Ask for serum calcium, phosphate, PTH, 25‑hydroxy vitamin D, and creatinine clearance. These numbers give a clear picture of how the kidney‑bone‑gut loop is functioning.

Really hope you get the right meds, its tough dealing with the gut issues.
People think kidney problems are just about blood, but the gut is the real battlefield. The hormone chaos is just a symptom of a failing system.
The so‑called medical literature on secondary hyperparathyroidism conveniently glosses over the fact that the entire gastrointestinal distress is nothing more than a deliberate side effect engineered by the pharmaceutical conglomerates.
They want you to believe that a simple phosphate binder will magically fix the gut, while in reality the binder itself is a thinly veiled vector for calcium overload.
Every time you take a calcium‑based binder you are feeding the very hormone surge that makes your intestines spasm.
The hidden agenda is obvious once you connect the dots between the rising rates of chronic kidney disease and the aggressive marketing of vitamin D analogs.
You are told to increase vitamin D intake, but the active forms are synthesized only in functional kidneys, which most of these patients lack.
Thus the industry pushes calcimimetics as a miracle solution, yet those drugs are manufactured under patents that prevent any real competition or transparency.
Meanwhile, the gut microbiome is deliberately sabotaged by excess phosphate, creating dysbiosis that fuels inflammation and further nutrient malabsorption.
The cascade of nausea, constipation, and reflux is not an unfortunate side effect but a predictable outcome of a system designed to keep you dependent on endless prescriptions.
If you scrutinize the lab values, you’ll notice that the recommended calcium thresholds are deliberately set at a level that masks early toxicity.
The same guidelines that tell you to "watch your diet" are written by committees that receive funding from the very manufacturers of the high‑phosphate processed foods they warn against.
It is no coincidence that soda consumption has skyrocketed in the same period that CKD-related hyperparathyroidism has become a public health nightmare.
The narrative that probiotics can "restore balance" is another puff‑piece, as most commercial probiotic strains are selected for survivability, not for any proven efficacy against phosphate‑driven bacterial overgrowth.
Patients who question this paradigm are often labeled as non‑compliant, and their concerns are dismissed as "mental health issues" in the medical notes.
This systematic marginalization serves to keep the status quo intact, ensuring that the profit margins of pharma remain untouched.
In short, the gut problems you experience are the predictable fallout of a broken feedback loop that the healthcare industry has a vested interest in preserving.
Awareness is the first step to breaking free from this engineered dependency, and the only way forward is to demand transparent research and truly independent treatment protocols.
Whoa, that's a wild ride of theories, but let’s bring it back to the science: high PTH does mess with smooth‑muscle tone, and phosphate overload can indeed shift the microbiome.
Still, most of what’s described in the article is backed by peer‑reviewed studies, not secret cabals.
Great summary! 👍 The probiotic tip really helped my friend who’s on phosphate binders. Keeping hydrated and adding fiber made a noticeable difference.
This is just another endless medical blurb.
The article correctly emphasizes monitoring serum calcium, phosphate, and PTH levels; without these labs, any dietary adjustment is speculative at best.
Oh sure, because “another endless medical blurb” is exactly what we needed to motivate patients to read more, right? 🙄 Anyway, if you actually look at the guidelines, they’re not rocket science.