Every week, pharmacies across the U.S. receive dozens of drug recall notices. Some are urgent. Some are false alarms. But if you miss one critical alert - the kind that warns about a contaminated blood pressure pill or a mislabeled insulin vial - someone could get seriously hurt. The system isn’t perfect. But if you know how to check for recall notifications the right way, you can stop errors before they reach patients.
Understand the Three Levels of Drug Recalls
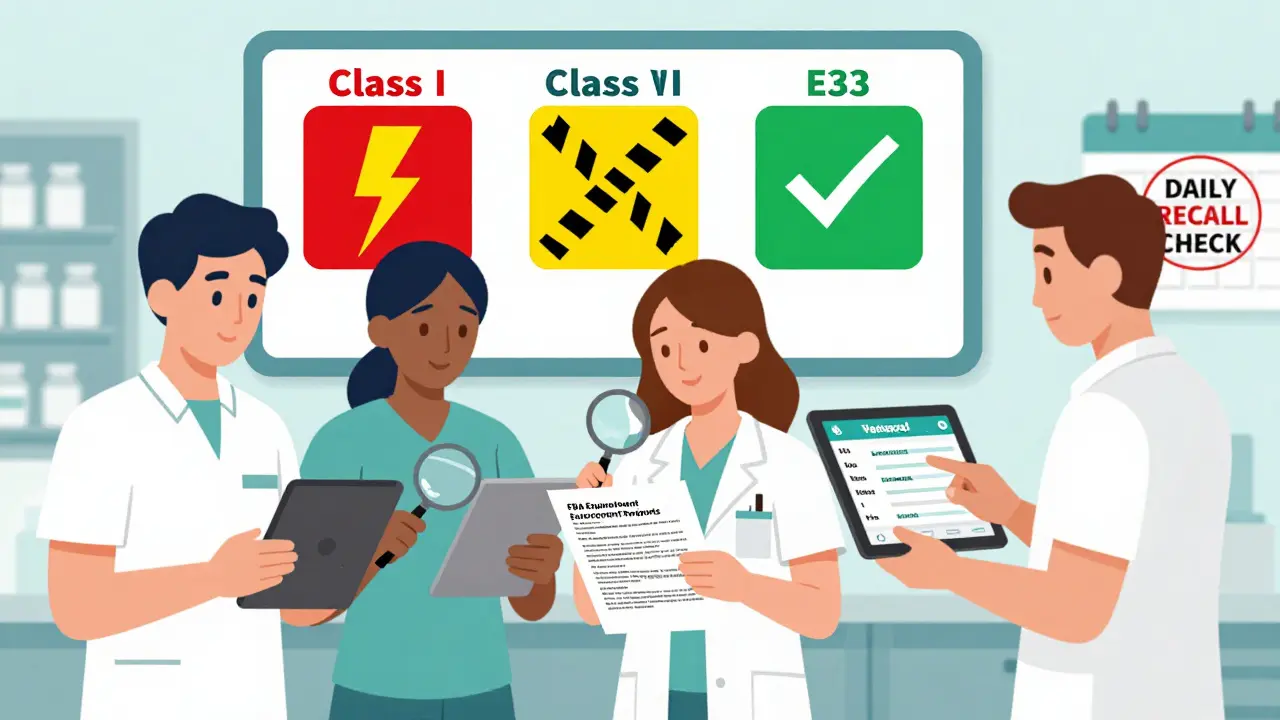
Not all recalls are the same. The FDA classifies them into three categories based on risk:- Class I: The most serious. These involve drugs that could cause serious injury or death. Think contaminated antibiotics, pills with wrong dosages, or unlabeled insulin. Response time: 24 hours or less.
- Class II: Drugs that might cause temporary health problems or pose a low risk of serious harm. Examples include misprinted labels or minor contamination. Response time: within 72 hours.
- Class III: Least serious. These are products that violate FDA labeling or manufacturing rules but won’t harm patients. Think incorrect expiration dates or packaging errors. Response time: within 2 weeks.
Class I recalls make up only about 4% of all notifications, but they demand immediate action. If your pharmacy gets one, you need to act fast - and you need to know you got the right notice.
Set Up Your Primary Notification Channels
You can’t rely on just one way to get recall alerts. The FDA and industry experts say pharmacies need at least three redundant systems. Here’s what works:- FDA MedWatch Email Alerts: Free. Sign up at www.fda.gov/Safety/MedWatch. You’ll get daily emails listing all new recalls, including lot numbers, NDC codes, and recall class. This is your baseline. Don’t skip it.
- Your Wholesaler’s System: Whether you buy from McKesson, Cardinal Health, or AmerisourceBergen, they all have automated recall systems. These are usually free for contract pharmacies. They send alerts via email, fax, or direct feed into your pharmacy software. Important: Wholesalers sometimes send false positives - like recalls for lots you never stocked. You still need to verify.
- Your Pharmacy Management System: This is the most powerful tool. Systems like QS/1, PioneerRx, and FrameworkLTC pull FDA data hourly and automatically flag matching lots in your inventory. If your system says “Lot #12345 of Metoprolol is recalled,” and you have that exact lot on the shelf - it lights up. No manual lookup needed.
According to a 2023 FDA study, pharmacies using integrated systems cut their recall response time from over 7 hours to under 1.5 hours. That’s the difference between a near miss and a real patient harm.
Verify Every Recall Within 4 Hours
Receiving a notice isn’t enough. You must verify it. Here’s how:- Check the recall classification. Is it Class I? Then you have 24 hours to act - but start immediately.
- Match the NDC and lot number. Every drug has a unique 11-digit NDC code. Cross-check it with your inventory. Don’t guess. Don’t rely on drug names alone. Two different brands of metoprolol can have different NDCs.
- Check your dispensing records. If the recall affects patients who already got the drug, you may need to notify them. Class I recalls require 100% patient notification. Class II needs 80%. The FDA requires you to document who you contacted and when.
- Confirm the recall is active. Sometimes recalls are withdrawn. Always check the FDA’s official Enforcement Reports - published every Wednesday - to confirm the notice hasn’t been lifted.
Pharmacists at independent shops report spending 3.2 hours per week just managing recalls. That’s why automation helps. But even with software, you still need to double-check. One pharmacy in Ohio missed a Class I recall in 2023 because their system didn’t flag a lot number that was formatted differently than their database expected. The FDA changed its format rules in 2024 - now all lot numbers must be 15 characters. If your system doesn’t handle that, it’s outdated.
Know Your System’s Weak Spots
Even the best tools have flaws. Here are the most common problems pharmacies face:- False positives: Wholesalers send recalls for lots you never ordered. You waste time checking them. Solution: Keep a log of your purchase history and cross-reference before acting.
- Missed notifications: Emails get filtered. Faxes jam. Staff forget to check. Solution: Set up a daily 10-minute recall check during morning shift change. Make it a ritual.
- Inventory access issues: Techs can’t pull up records after hours. If a recall hits at 8 p.m., and your system locks out after 6 p.m., you’re vulnerable. Solution: Ensure your pharmacy software allows remote access for verified staff.
- Sync programs: Patients on medication synchronization get 90-day supplies. A recall on a 30-day pill might miss 60 days’ worth of meds already dispensed. The Institute for Safe Medication Practices says 43% of Class I recalls miss these patients. You need to track sync patients separately.
Independent pharmacies struggle most. PioneerRx’s recall module costs $2,495 a year plus $495/month for data feeds. If you only get 2-3 recalls a year, it feels like overkill. But one missed Class I recall can cost you more than that in lawsuits, fines, and lost trust.
Train Your Team and Document Everything
Recall response isn’t just the pharmacist’s job. It’s a team effort. The ASHP recommends forming a Recall Response Team with at least two people trained and available 24/7 for Class I events. Training takes 8 hours initially, then 2 hours every quarter.Here’s what your team needs to know:
- How to access FDA MedWatch and your wholesaler’s portal
- Where to find NDC codes on your inventory screen
- How to generate a patient list for recall notifications
- When to call patients vs. send letters
Documentation is non-negotiable. The FDA requires you to keep recall records for 3 years. That includes:
- When you received the alert
- Which lots you confirmed
- How many units you quarantined
- Which patients you contacted
- Proof of notification (call logs, letters, emails)
92% of pharmacies now use electronic audit trails. If you’re still using paper logs, you’re at risk during inspections. CMS will start requiring proof of recall response capability during Medicare accreditation surveys starting in 2024.

What’s Changing in 2025 and Beyond
The system is getting smarter - but only if you keep up.- HL7 data standards: By December 2025, all FDA recall data must be sent in structured XML format. This will let pharmacy systems auto-match lots without human input.
- Blockchain pilots: The MediLedger Project, now testing with 12 manufacturers and 3 pharmacy chains, lets pharmacies trace every pill back to its batch in seconds. It’s not everywhere yet, but it’s coming.
- AI verification: University of Florida’s pilot showed AI tools can reduce manual review time by 68%. By 2025, most hospital pharmacies will use them. Community pharmacies will follow.
- Patient risk data: Starting January 2025, Class I recalls must include patient-level risk assessments. That means you’ll get not just “this lot is bad,” but “this lot was given to 12 elderly patients with kidney disease.”
By 2027, experts predict manual recall checks will be obsolete. The system will auto-quarantine bad lots, notify patients, and update inventory - all in minutes.
Bottom Line: Don’t Wait for a Crisis
You don’t need fancy tech to start. But you do need a plan.- Sign up for FDA MedWatch today - it’s free.
- Confirm your wholesaler sends recall alerts - and test them.
- Check your pharmacy software: Does it auto-flag recalled lots? If not, ask your vendor.
- Train your staff. Make recall checks part of your daily routine.
- Document everything. You’ll thank yourself if the FDA ever asks.
Drug recalls aren’t going away. But with the right systems, you can turn a potential disaster into a routine check. That’s not just good practice - it’s what keeps patients safe.


This whole guide is just corporate fluff. The FDA doesn't care about your little pharmacy. They're busy protecting Big Pharma's profits. I've seen recalls get buried for months while the same toxic pills keep circulating. You think signing up for MedWatch helps? It's a trap. They feed you noise so you stop looking for the real problems.
I've been doing this for 18 years. The system is broken but you're right - automation saves lives. My team used to spend 12 hours a week chasing false alerts. Now it's under 90 minutes. The software doesn't replace judgment, but it frees you to use it.
Ah, the sacred ritual of the recall check - a modern-day sacrament performed by altar boys in scrubs. We've turned patient safety into a liturgy of compliance, where the holy texts are NDC codes and the priests are QA coordinators with quarterly training certificates. The real tragedy? We've forgotten that medicine is about human beings, not barcodes and audit trails. The soul of pharmacy has been outsourced to HL7 XML schemas.
Love this breakdown. We just implemented FrameworkLTC last month and holy crap it changed everything. Used to miss two recalls a year because someone forgot to check the email. Now it lights up like a Christmas tree. My techs actually cheer when a recall pops up because they know it means they're doing their job right
They're lying. All of it. The FDA, the wholesalers, the software companies - they're all in on it. That 'Class I' recall you think you caught? It was planted. They want you to panic so you buy more of their expensive software. And don't get me started on blockchain - it's just the NSA with better PR. They're tracking every pill you touch.
In India we don't have fancy systems like this but we still save lives. We talk to patients. We know their names. We remember if Mrs. Patel takes metoprolol for her husband who passed last year. We don't need NDC codes to know when something's wrong. We just look in their eyes. Your tech is cool but it's not replacing human connection. Maybe you're missing the point.
You mention '2027' like it's some utopian future. But you're ignoring the real crisis: pharmacies are being turned into warehouses for corporate greed. You're celebrating automation while ignoring that the average pharmacist now spends 80% of their day clicking buttons instead of counseling patients. This isn't progress - it's dehumanization dressed up as safety. And you call this a 'guide'? It's a corporate manual for surrender.
Fascinating. So we're to believe that a system which failed to detect the 2022 heparin contamination, the 2023 valsartan NDMA scandal, and the 2024 metformin recall - all of which originated from unregulated overseas manufacturers - is now somehow 'self-correcting' through HL7 and blockchain? The irony is thick enough to spread on toast. The real innovation here is the ability to outsource blame to software.
This is why America is falling apart. We let foreign labs make our pills and then we pay $5,000 a year to software companies to tell us when they poisoned us. The FDA is a joke. They take money from the same companies they're supposed to regulate. I'd rather trust my local pharmacist who knows my grandma's meds than some robot that can't even spell 'lot number' right.
I applaud the thoroughness of this guide. However, I must emphasize that the integration of blockchain-based traceability, as proposed under the MediLedger Project, must be accompanied by mandatory interoperability standards across all pharmacy management systems. Without a unified data schema - preferably adhering to ISO 15189:2022 - we risk creating fragmented silos that undermine the very integrity of recall responsiveness. Furthermore, the documentation protocols outlined require alignment with HIPAA 2025 amendments regarding patient notification audit trails. This is not merely operational - it is a fiduciary imperative.
We rolled out the MediLedger pilot last quarter. The real win? We caught a Class II recall before it even hit our shelves because the manufacturer’s batch ID was flagged in the chain. No email. No alert. Just a silent blockchain verification. The tech’s not magic - it’s just better than waiting for a fax to jam. Still, nothing beats a pharmacist who actually knows their patients’ meds by heart.
You people are naive. You think a software update fixes everything? The FDA has been compromised since 2019. The same people who approve the drugs are the ones who write the recall notices. And you're paying for this? You're paying for a system that lets them keep selling dangerous drugs - and then you pat yourselves on the back for checking the right box. This isn't safety. It's theater. And you're the audience.
I read this entire thing. Took me 22 minutes. I'm still not sure if it's a guide or a sales pitch for PioneerRx. Either way, the fact that you need to spend $3,000 a year just to avoid killing someone is a moral failure. My cousin works at a rural pharmacy in West Virginia. They use Excel. They print emails. And they've never missed a recall. Sometimes the oldest way is the only honest one.
I work in a pharmacy. We got a recall last week. The software said 'Lot 12345' - but the label on the bottle said 'LOT12345' - no space. The system didn't catch it. We found it because the tech noticed the label looked weird. So your 'auto-flagging' system? It's useless. And now I'm supposed to trust AI? I'll trust my eyes before I trust a machine that can't read a space.
This guide is exemplary in its rigor and clarity. The structured delineation of recall tiers, coupled with the emphasis on redundant verification protocols, reflects a profound commitment to patient safety that is increasingly rare in contemporary healthcare practice. The integration of FDA MedWatch with institutional pharmacy management systems constitutes a paradigmatic shift toward evidence-based pharmacovigilance. I would urge all stakeholders to adopt these protocols without delay, as noncompliance constitutes a breach of the ethical duty of nonmaleficence. Documentation is not bureaucracy - it is accountability incarnate.