Every year, hundreds of thousands of people end up in the hospital not because their illness got worse, but because they took two medications at the same time. It’s not always about dosage or allergies. Sometimes, it’s just about timing.
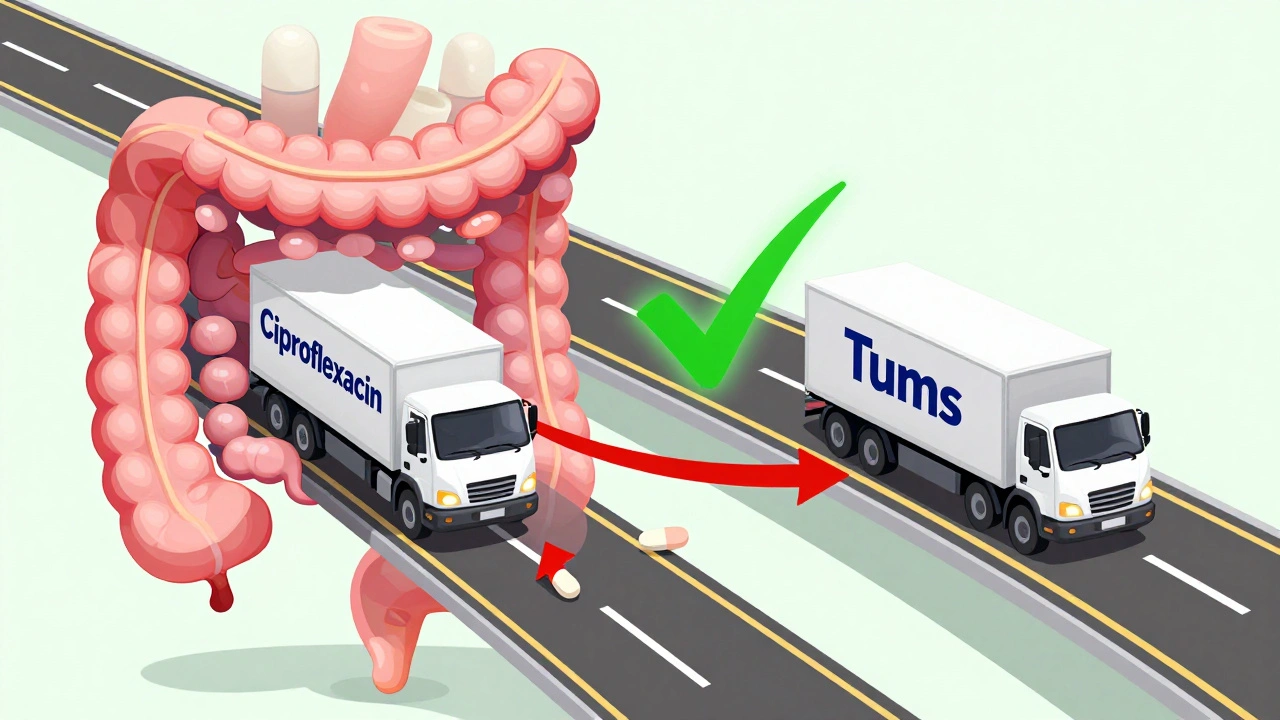
Take ciprofloxacin, a common antibiotic. If you take it with an antacid like Tums or Maalox, your body absorbs almost 90% less of the antibiotic. That means the infection might not clear up - and could even get worse. But if you wait just two hours between the two, the problem disappears. No dose change. No switch to a different drug. Just better timing.
This isn’t rare. About 1 in 5 of all drug interactions you hear about in hospitals can be fixed by spacing out when you take your pills. That’s the power of time-dependent drug interactions - or TDDIs. These aren’t random accidents. They’re predictable, preventable, and often overlooked.
Why Timing Matters More Than You Think
Most people think drug interactions mean one pill cancels out another. But that’s not always true. Sometimes, one drug just gets in the way of another being absorbed.
Imagine your stomach and intestines as a highway. Some drugs are like trucks that block the road. Antacids raise stomach pH, which stops antibiotics like ciprofloxacin or tetracycline from being absorbed. Iron supplements and calcium pills do the same thing to thyroid meds like levothyroxine. If you take them together, your body might only get 5% of the dose you paid for.
Studies show that levothyroxine absorption drops from 95% to under 50% when taken with iron or calcium within 4 hours. That’s enough to throw your thyroid levels off - leading to fatigue, weight gain, or even heart problems. But if you take your thyroid pill first thing in the morning on an empty stomach, and wait four hours before taking your calcium or iron, your levels stay stable.
It’s not just absorption. Some drugs change how fast your liver breaks down others. But here’s the catch: if it’s a liver metabolism issue - like warfarin and metronidazole - timing won’t help. You can’t out-schedule your liver. Those need dose changes or different drugs entirely. Timing only works when the problem happens in your gut, not your bloodstream.
Which Medications Need Separation - And How Long?
Not all drugs need spacing. But a lot of the ones people take daily do. Here are the most common ones and the exact time gaps that work:
- Levothyroxine - Wait 4 hours before taking iron, calcium, magnesium, or aluminum-containing products (like antacids or supplements).
- Fluoroquinolones (ciprofloxacin, levofloxacin) - Separate from antacids, dairy, or multivitamins with zinc/iron by at least 2 hours.
- Tetracycline antibiotics - Don’t take with milk, calcium, or antacids. Wait 3 hours before or after.
- Bisphosphonates (alendronate, risedronate) - Take on empty stomach with plain water. Wait 30 minutes before eating, drinking, or taking anything else.
- Proton pump inhibitors (PPIs like omeprazole) - Avoid taking with iron or vitamin B12 supplements within 2 hours. PPIs lower stomach acid, which reduces absorption of these nutrients.
- Clarithromycin and colchicine - Separate by 2 hours to reduce risk of dangerous muscle toxicity, especially in older adults.
These aren’t guesses. They’re based on clinical studies published in journals like the Journal of Clinical Endocrinology & Metabolism and FDA labeling guidelines. The numbers matter. Two hours isn’t enough for levothyroxine. Four hours is the minimum. And for bisphosphonates, 30 minutes isn’t optional - it’s required.
What Timing Can’t Fix
Timing is powerful, but it’s not magic. Some interactions are built into how your body works - and you can’t outwait them.
Take warfarin and NSAIDs like ibuprofen. Both thin your blood. Taking them together increases bleeding risk - no matter when you take them. The same goes for statins and grapefruit juice. Grapefruit blocks an enzyme in your liver that breaks down statins. That means too much drug stays in your system, raising the risk of muscle damage. You can’t time around that. You have to switch to a different statin or avoid grapefruit entirely.
Another example: metronidazole and alcohol. Even if you take them 6 hours apart, the reaction still happens. Your body processes them together, creating a toxic compound. That’s a pharmacodynamic interaction - not absorption-based. Timing doesn’t help. Only avoidance does.
That’s why knowing the type of interaction matters. If the problem is absorption - timing helps. If it’s metabolism, enzyme blocking, or additive effects - you need a different plan. Always check with your pharmacist or doctor before assuming timing will fix everything.

Real-Life Successes - And Failures
At a geriatric clinic in San Francisco, pharmacists started tracking when patients took their iron and PPIs. They noticed a pattern: people on both were still anemic. So they created a simple rule: take iron in the morning, PPI at lunch, and nothing else for 2 hours after. Within 18 months, iron deficiency cases dropped by 32%.
But not all stories end well. A nurse in Boston surveyed patients on 10 or more medications. Nearly 40% couldn’t follow their timing schedule. Why? Too many rules. Too many colors on their pill organizer. Too many different times. One 78-year-old woman told her, “I forget which one I’m supposed to wait for. I just take them all when I wake up.”
That’s the hidden problem: complexity kills adherence. If your schedule looks like a spreadsheet, you’re not going to stick to it. The best solutions are simple: one pill first thing in the morning, wait 30 minutes, then breakfast. Another pill at bedtime, with no food or supplements for 2 hours before. Consistency beats perfection.
How to Get Started - Step by Step
If you’re on more than three medications, here’s how to start fixing your timing:
- Write down everything you take - pills, vitamins, supplements, even herbal teas. Don’t skip anything.
- Look for the big offenders - antacids, calcium, iron, thyroid meds, antibiotics. These are the most common culprits.
- Check the timing rules - Use trusted sources like Lexicomp, Micromedex, or ask your pharmacist. Don’t rely on Google.
- Build a simple schedule - Group meds that can be taken together. Separate the ones that need space. Use a color-coded chart or app like Medisafe.
- Test it for a week - Stick to the plan. Note if you feel better, have fewer side effects, or notice changes in energy or digestion.
Most people can do this in 20 minutes. But it’s not a one-time fix. Your meds change. Your doctor adds something. You start a new supplement. Revisit your schedule every time your prescription changes.

Tools That Actually Help
You don’t need fancy gadgets. But a few simple tools make a huge difference:
- Multi-compartment pill organizer - Buy one with AM/PM/Evening slots. Label each compartment with the time. Studies show this cuts timing errors by 43%.
- Medisafe or MyTherapy app - Set custom alerts for each med with a 15-minute buffer. These apps send reminders and even tell you when to wait.
- Pharmacist consultation - Most pharmacies offer free med reviews. Ask them: “Which of my meds need spacing?” They’ll give you a printed list.
Don’t rely on your memory. Even smart people forget. A 2021 study with over 1,200 patients showed that those using timing alerts in an app improved adherence by 57%. That’s not just helpful - it’s life-saving.
When to Call Your Doctor
Timing helps - but it’s not always enough. Call your doctor if:
- You’re still having side effects even after spacing your meds.
- You’re taking more than five medications daily.
- You’ve been hospitalized for a drug reaction before.
- You’re over 65 and taking multiple prescriptions.
Some interactions can’t be fixed by timing. You might need a different drug, a lower dose, or a different form (like a liquid instead of a pill). Don’t be afraid to ask: “Is there a safer way to take this?”
Medication timing isn’t about being perfect. It’s about being smart. It’s about using what we already know to keep you safe - without adding more pills or more costs. And in a world where drug interactions are one of the top causes of preventable hospital stays, that’s not just helpful. It’s essential.
Can I take my vitamins with my morning medications?
It depends. If your vitamins contain calcium, iron, or magnesium, don’t take them with thyroid meds, antibiotics, or bisphosphonates. Wait at least 2-4 hours. If your vitamin is just a basic multivitamin without those minerals, it’s usually fine. Always check the label or ask your pharmacist.
What if I forget and take two meds together?
Don’t panic. Skip the next dose only if your doctor or pharmacist says so. For most absorption-based interactions, missing one dose won’t cause harm - but it might reduce effectiveness. Don’t double up. Just get back on schedule. If you’re unsure, call your pharmacy. They’re used to this.
Does it matter if I take my meds with food?
Yes - and it depends on the drug. Levothyroxine and bisphosphonates must be taken on an empty stomach. Antibiotics like tetracycline are less effective with dairy. But some meds, like statins or blood pressure pills, work better with food. Always follow the label. If it says “take on empty stomach,” wait 30-60 minutes before eating.
Why do some drug labels not mention timing?
Many older labels don’t include timing details because they were approved before this science was widely understood. The FDA now requires timing instructions for 27% more drugs than in 2018, but not all have been updated. If you’re unsure, don’t guess. Ask your pharmacist - they have access to the latest interaction databases.
Can I use a pill organizer with timed compartments?
Yes - and it’s one of the best tools you can use. Look for organizers with separate compartments for morning, afternoon, evening, and bedtime. Label each one clearly. Avoid ones with too many tiny slots - they can cause confusion. A simple 4-compartment box with clear labels reduces timing errors by nearly half.
Is medication timing only for older adults?
No. While older adults are more likely to take multiple medications, anyone on more than three drugs daily can benefit. Younger people on antibiotics, birth control, thyroid meds, or supplements also face timing issues. It’s about the number and type of meds - not age.
If you’re managing several medications, start today. Write down your list. Check one interaction. Wait two hours next time. Small steps prevent big problems.

bro i took my cipro with a gummy vitamin and now i feel like a zombie. like, why does this shit even exist? i thought meds were supposed to help, not turn you into a confused potato. 🤡
I CAN'T BELIEVE PEOPLE DON'T KNOW THIS. I've been a nurse for 18 years and I STILL see patients taking levothyroxine with their calcium supplement at breakfast. It's not just stupid-it's dangerous. 🙄
The data here is solid. Absorption-based TDDIs are grossly under-discussed in clinical practice. The 90% reduction in ciprofloxacin bioavailability when co-administered with divalent cations is well-documented in FDA labeling (2020 update) and confirmed by multiple RCTs. This isn't anecdotal-it's pharmacokinetic law. 📊
I just started taking levothyroxine and I was so overwhelmed. This post literally saved me. I didn’t know I had to wait 4 hours for my iron. I used to take them together because I was tired in the morning. Now I set an alarm. I feel better already. Thank you.
This is the kind of practical, science-backed info we need more of. I’ve seen too many people panic over drug interactions when a simple 2-hour buffer solves everything. Also, props for mentioning pharmacists-they’re the real MVPs. 🙌
Wait-so you’re telling me I’ve been taking my PPI and iron together for TWO YEARS?!?!?!?!? I’m 52, have low ferritin, and my doctor never told me?!? I’m filing a complaint. This is malpractice. 😡
i just take everything at night. works fine. why make it so complicated? i don't care about all this science stuff. my body's fine.
In India, many patients take antibiotics with milk due to cultural habits. This post is a wake-up call. I shared it with my elderly aunt who takes levothyroxine and calcium. She now waits 4 hours. Her TSH normalized in 6 weeks. 🙏
You don’t need to be perfect. Just start with ONE thing. Pick your worst combo. Wait two hours. Do it for a week. That’s it. You got this. 💪
This is fascinating from a pharmacological standpoint. The gut as a highway metaphor is actually quite apt-absorption is a dynamic process influenced by pH, motility, and transporter saturation. The 2-hour window for fluoroquinolones aligns with gastric emptying kinetics, and the 4-hour separation for levothyroxine correlates with the time needed for gastric pH to return to baseline after antacid use. The real challenge, however, is adherence in polypharmacy populations. Even with perfect knowledge, cognitive load and memory deficits in the elderly create systemic barriers. Perhaps the solution isn’t just education, but automated dispensers with timed compartments and pharmacist-led reconciliation at every visit. This needs to be institutionalized, not left to individual discipline.
yo i just took my antibiotic with my protein shake and now i feel weird. is this bad? 🤔
It’s funny how we treat our bodies like machines you just plug into, but forget they’re ecosystems. Timing isn’t about rules-it’s about listening. The body doesn’t care about your schedule. It cares about rhythm. Maybe the real lesson isn’t when to take your pills… but when to slow down and pay attention.