Beta-Blocker Safety Checker
Select the beta-blocker you're taking to understand your hypoglycemia risk and get personalized safety recommendations.
Your Risk Assessment:
Recommended Actions:
When you're managing diabetes with insulin, your body depends on a delicate balance. Too much insulin, and your blood sugar drops dangerously low-hypoglycemia. Now add a beta-blocker, commonly prescribed for high blood pressure or heart conditions, and things get riskier. You might not even know your blood sugar is crashing. This isn’t a rare edge case. It’s a well-documented, life-threatening interaction that affects thousands of people every year.
Why Beta-Blockers Hide Low Blood Sugar
Beta-blockers don’t make your blood sugar drop on their own. But they silence the alarms your body uses to warn you it’s happening. When your glucose falls, your nervous system kicks in: your heart races, your hands shake, you break out in a cold sweat. These are your body’s natural warning signs. Beta-blockers block the adrenaline response, so your heart doesn’t race and your hands stop trembling. That sounds helpful for heart patients-but for someone on insulin, it’s dangerous.
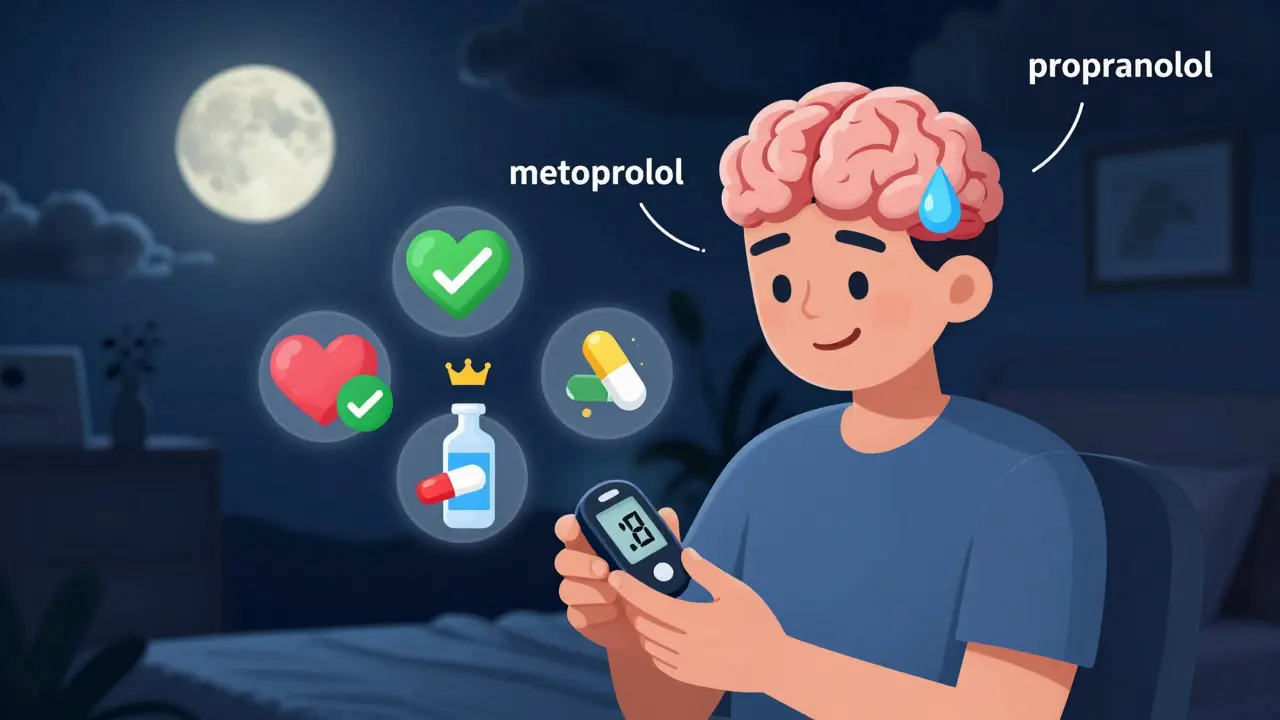
Here’s the catch: not all beta-blockers are the same. Non-selective ones, like propranolol, block both beta-1 and beta-2 receptors. That means they wipe out nearly all physical warning signs. Even cardioselective beta-blockers, like metoprolol or atenolol, which mainly target the heart, still reduce or eliminate tremors and palpitations. The one warning sign they usually don’t touch? Sweating. That’s because sweating is triggered by acetylcholine, not adrenaline. If you’re on insulin and a beta-blocker, sweating is your last line of defense.
The Real Danger: Hypoglycemia Unawareness
Hypoglycemia unawareness isn’t just missing a shaky hand or fast heartbeat. It’s when your brain stops recognizing low sugar altogether. You go from feeling fine to confused, disoriented, or unconscious-with no warning. This happens in about 40% of people with type 1 diabetes, and less often in type 2, but the risk spikes dramatically when beta-blockers are added.
Studies show that patients on insulin and beta-blockers are 2.3 times more likely to have a hypoglycemic event in the hospital. And here’s the scariest part: 68% of those events happen within the first 24 hours of starting or changing the beta-blocker. That’s why hospitals now require blood glucose checks every 2 to 4 hours for diabetic patients on these medications.
It’s not just about feeling bad. Severe hypoglycemia can trigger heart arrhythmias, seizures, strokes, or death. Research from Dungan’s 2019 study found that hypoglycemia increased hospital mortality by 3.2 times in patients on selective beta-blockers. And for those with hypoglycemia unawareness? The risk of death from low blood sugar rose by 28% compared to those not on beta-blockers.
Carvedilol: The Safer Choice?
Not all beta-blockers are created equal when it comes to diabetes. Carvedilol stands out. Unlike metoprolol or atenolol, carvedilol has additional properties-it blocks alpha receptors and has antioxidant effects. More importantly, studies show it’s less likely to mask hypoglycemia symptoms. The 2022 American College of Cardiology guidelines noted a 17% reduction in severe hypoglycemia events when carvedilol was used instead of metoprolol in diabetic patients.
Even better, carvedilol doesn’t carry the same mortality risk. Dungan’s research found that patients on carvedilol had an odds ratio of 0.78 for hypoglycemia-related death-meaning they were actually less likely to die from low blood sugar than those not on any beta-blocker. That’s not a typo. Carvedilol might be the safest beta-blocker option for people with diabetes who need heart protection.

How to Stay Safe: Practical Steps
If you’re on insulin and a beta-blocker, here’s what you need to do:
- Check your blood sugar more often. Aim for at least every 4 hours, especially in the first few days after starting the beta-blocker. At night, check before bed and if you wake up feeling odd.
- Know your one real warning sign: sweating. If you break out in a cold sweat for no reason, treat it like low blood sugar-even if your meter says you’re fine. Glucose levels can drop fast.
- Avoid non-selective beta-blockers. Stay away from propranolol, nadolol, or timolol if you have a history of low blood sugar or unawareness.
- Use a continuous glucose monitor (CGM). Since 2018, CGM use has jumped 300% among patients on beta-blockers. Why? Because it catches drops before you feel them. Studies show CGMs reduce severe hypoglycemia by 42% in this group.
- Teach your family or roommate. If you lose consciousness during a low, they need to know to give you glucagon or call 911. Don’t assume they’ll know what to do.
What About Long-Term Risk?
You might hear conflicting things. The ADVANCE trial, which tracked over 11,000 diabetic patients for five years, found no significant difference in severe hypoglycemia rates between those on atenolol and those on placebo. That suggests outpatient risk might be lower than hospital risk. But here’s the thing: hospitals are high-stress environments. People eat irregularly, get sick, get IV fluids, and have medication changes. That’s when the danger spikes.
Outside the hospital, if you’re consistent with meals, monitoring, and insulin doses, your risk stays lower. But that doesn’t mean it’s gone. Hypoglycemia unawareness can still creep in over time-especially if you’ve had frequent lows in the past. Your brain gets used to low sugar and stops sounding the alarm.
The Bigger Picture: Heart vs. Blood Sugar
This is the hardest part. Beta-blockers save lives. After a heart attack, they cut post-MI death risk by 25%. For people with diabetes-who already have 2 to 4 times higher risk of heart disease-stopping a beta-blocker can be deadly. You can’t just quit them because of hypoglycemia risk.
The goal isn’t to avoid beta-blockers. It’s to use them smarter. Choose carvedilol if possible. Monitor closely. Use CGM. Educate yourself. Work with your doctor to find the lowest effective dose. The American Heart Association and the American Diabetes Association both agree: don’t stop the beta-blocker. Optimize the safety around it.
What’s Next? Personalized Medicine
Researchers are now looking at genetics. The 2023 DIAMOND trial is testing whether certain gene variants make some people more likely to develop hypoglycemia unawareness when on beta-blockers. If successful, we could one day test a patient’s DNA before prescribing a beta-blocker-and choose the safest option based on their biology.
Until then, the best tools we have are awareness, monitoring, and smart drug choices. Don’t assume you’re fine just because you don’t feel shaky. Sweat is your friend. Your glucose meter is your lifeline. And carvedilol might be the best beta-blocker for your heart-and your blood sugar.
Can beta-blockers cause low blood sugar on their own?
No, beta-blockers don’t directly lower blood sugar. But they prevent your body from signaling when it’s dropping, and they can interfere with the liver’s ability to release glucose. This makes hypoglycemia more likely and harder to detect-especially when combined with insulin.
Is it safe to take beta-blockers if I have type 2 diabetes?
Yes, but with caution. While hypoglycemia unawareness is less common in type 2 than type 1, it still happens-especially if you’re on insulin or sulfonylureas. Always monitor glucose closely, especially when starting or changing beta-blockers. Carvedilol is preferred over metoprolol or atenolol.
What should I do if I feel fine but my CGM shows a low?
Treat it. Even if you feel perfectly normal, a low reading means your body is in danger. Your brain may no longer be sensing the drop. Eat 15 grams of fast-acting carbs, recheck in 15 minutes, and don’t drive or operate machinery until your sugar is stable.
Can I switch from metoprolol to carvedilol?
Talk to your doctor. Switching beta-blockers isn’t automatic. Your heart condition, kidney function, and current dose matter. But if you’re on insulin and have had lows or unawareness, carvedilol is often a better choice. Studies show it lowers hypoglycemia risk by 17% compared to metoprolol.
Do I need to stop my beta-blocker if I start using a CGM?
No. CGMs don’t replace the need for careful beta-blocker management-they enhance it. CGMs give you real-time data, so you can catch lows before they become emergencies. Continue your beta-blocker, but use the CGM as your new early-warning system.


Let me tell you something they don’t want you to know. Beta-blockers? Totally a Big Pharma scam to keep diabetics dependent on CGMs and glucagon pens. I read a paper once - buried in a journal no one cites - that said the real reason they hide hypoglycemia is because it creates more data points for insurance billing. You think sweating is your last warning sign? Nah. It’s the algorithm. They’re tracking your glucose drops to upsell you on ‘premium’ insulin pumps. I’ve stopped taking mine. My blood sugar’s never been better. #WakeUp
OMG this is so true 😭 I’ve been on metoprolol for 3 yrs and my sugar keeps dropping like im in a elevator with no brakes 🤯 I thought I was just bad at diabetes but now I realize its the beta blocker!! I switched to carvedilol last month and my CGM stopped screaming at me at 3am!! I’m not saying I’m cured but my nights arent nightmares anymore 🙌 #DiabetesWarrior #CarvedilolIsLife
Check your sugar. Know your sweat. Use a CGM. Talk to your doctor. That’s it.
It is imperative to recognize that the confluence of insulin therapy and beta-blockade represents not merely a pharmacological interaction, but a profound physiological recalibration of autonomic signaling. The body’s innate homeostatic mechanisms - evolved over millennia - are being systematically dampened by synthetic compounds designed for cardiac stability. In this context, the human organism becomes a site of competing imperatives: the imperative to preserve cardiac function versus the imperative to preserve neurological integrity. The solution lies not in abandonment, but in nuanced, individualized therapeutic architecture - one that prioritizes vigilance, technological augmentation, and an unwavering commitment to patient autonomy.
Carvedilol changed my life. No more scary nights. I didn’t even know I was having lows until my CGM beeped. Now I just shrug and eat a juice box. Easy.
I’ve been on insulin for 18 years and beta-blockers for 6. I used to think I was just ‘bad at managing’ - until I had that one night where I woke up in the ER with no memory of how I got there. I didn’t shake. I didn’t sweat. I just… stopped. That’s when I realized hypoglycemia unawareness isn’t a symptom - it’s a silent thief. Since switching to carvedilol and getting a CGM, I’ve slept through the night for the first time in a decade. I didn’t know how much I was living in fear until I stopped. I wish someone had told me this sooner.
My doc put me on metoprolol. 3 days later I passed out in the grocery store. No warning. Just gone. Now I check my sugar every 2 hours. Even if I feel fine. Even if I’m on the toilet. Even if I’m kissing my girlfriend. I don’t care. I’m alive. That’s the win.
i just started carvedilol last week and my cgms been quiet at night 😌 i used to wake up drenched in sweat and panicking… now i just roll over. its weird how something so simple can feel like a miracle
Oh, so now we’re recommending carvedilol like it’s the new avocado toast? 😏 I’ve got a friend on it - he’s also vegan, meditates daily, and swears by Himalayan salt. Coincidence? I think not. But honestly? I’m glad someone’s finally talking about this. My uncle died from a low that nobody saw coming. We thought he was just ‘sleeping too hard.’