When a family qualifies for Medicaid or CHIP, they’re supposed to get help when they need it. But what if they already have private insurance? That’s where Medicaid substitution rules come in. These rules aren’t about denying care-they’re about making sure public funds aren’t used to replace coverage that’s already available and affordable. The federal government set these rules to protect private insurance markets and keep Medicaid focused on those who truly have no other options. But how they’re applied? That’s where things get messy-and wildly different-from state to state.
What Exactly Are Medicaid Substitution Rules?
Medicaid substitution rules come from Section 2102(b)(3)(C) of the Social Security Act, updated in 1997 and again in 2010 under the Affordable Care Act. The idea is simple: if a child has access to affordable private health insurance through a parent’s job, Medicaid or CHIP shouldn’t step in as the first option. The goal isn’t to punish families-it’s to prevent a situation where employers drop coverage because they know the government will pay for it instead.
These rules apply mostly to CHIP, the Children’s Health Insurance Program, which serves kids in families that earn too much for Medicaid but still can’t afford private plans. But the same logic affects Medicaid in states where eligibility overlaps. The key phrase here is “affordable private coverage.” That means a job-based plan where premiums don’t exceed 9.12% of household income in 2024, according to IRS guidelines. If it’s cheaper than that, Medicaid can’t automatically take over.
Mandatory Rules: What All States Must Do
Every state, plus Washington, D.C., is required by federal law to have a system in place to prevent Medicaid and CHIP from replacing private insurance. That’s non-negotiable. The core rule? States must verify whether a child has access to affordable group health coverage before enrolling them in CHIP. They can’t just assume.
States must also handle transitions smoothly. If a child loses job-based coverage, they can’t be stuck in a coverage gap while waiting for Medicaid to kick in. The 2024 CMS rule (CMS-2441-F), which took effect April 29, 2024, pushed states to create automatic transitions between Medicaid and CHIP when eligibility changes. That means if a parent’s income drops and they qualify for Medicaid, their child should move over without paperwork delays.
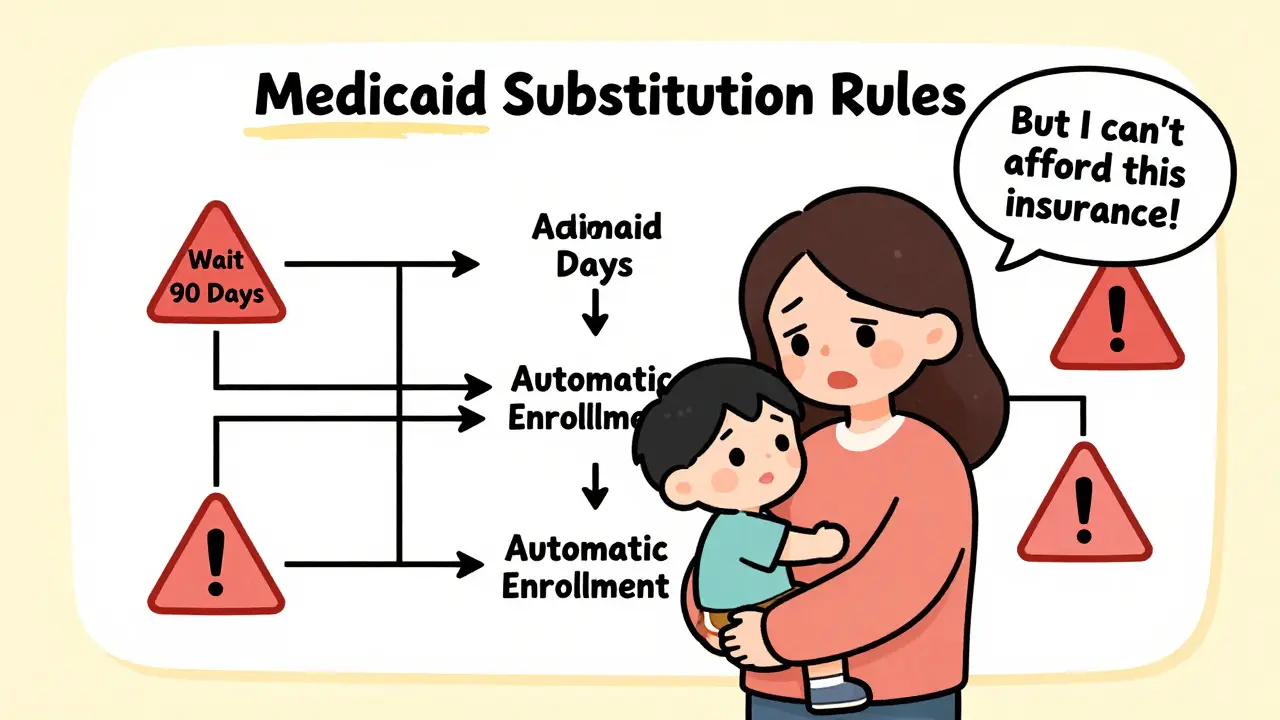
Another mandatory piece? States must allow exemptions to waiting periods. For example, if a parent loses a job, the state must still enroll the child in CHIP-even if they’d normally have to wait 90 days. That’s not optional. It’s a federal requirement to avoid leaving kids uninsured during sudden life changes.
Optional Rules: Where States Get to Choose
Here’s where things get complicated. While the core rule is mandatory, states have a lot of freedom in how they enforce it. The biggest choice? Whether to use a waiting period.
Up to 90 days is allowed under federal rules. Thirty-four states use this waiting period as their main tool to prevent substitution. That means if a family has access to private insurance-even if they didn’t sign up for it-they can be denied CHIP for up to three months. California, Texas, and New York are among the biggest states using this method. But here’s the catch: those 90 days aren’t always filled with coverage. A Medicaid worker in Ohio told a Reddit thread in 2023 that families often end up completely uninsured during that time because they can’t afford to pay for private insurance and can’t get public help yet.
Meanwhile, 16 states skip the waiting period entirely. Instead, they rely on real-time data systems to check whether private insurance is actually being used. These states monitor whether a child is enrolled in a group plan, whether premiums are being paid, and whether the coverage meets affordability standards. Twenty-eight states use private insurance databases for this, while 22 still rely on paper forms and household surveys-which can take weeks to process.
Another optional move? Adding extra exemptions. Fifteen states go beyond the federal minimum. Florida, Illinois, and Pennsylvania, for example, let families skip the waiting period if a parent’s hours are cut, if they’re in a seasonal job, or if they’re in the middle of a job transition. These states recognize that today’s workforce doesn’t follow the old 9-to-5, year-round model.

Why Some States Succeed-and Others Don’t
Not all states handle substitution the same way-and the results show it. States with integrated Medicaid-CHIP systems (32 as of 2024) have 22% fewer coverage gaps than those with separate systems. Why? Because when eligibility systems talk to each other, transitions happen faster.
Minnesota’s “Bridge Program” is a standout. By connecting private insurer data directly with public program databases, they cut substitution-related coverage gaps by 63%. Kids don’t fall through cracks. Parents don’t have to chase paperwork. It’s automated, real-time, and works.
On the flip side, Louisiana’s strict 2021 policy backfired. By making verification harder and waiting periods longer, the state saw its uninsured child rate jump by 4.7 percentage points in just one year. The Urban Institute called it a textbook example of how rigid rules can hurt the very people they’re meant to protect.
States that rely on paper forms and manual checks are struggling. In a 2023 survey of 47 state Medicaid agencies, 68% said verifying private insurance was their biggest headache. The average time to confirm coverage? 14.2 days. That’s longer than the average job search in many industries.
The Human Cost of Bureaucracy
Behind every rule is a family trying to survive. A parent working two jobs, one with insurance that’s too expensive to afford, the other with no benefits. They’re told they don’t qualify for CHIP because “you had access to coverage.” But what if that coverage was a $600/month premium on a $3,000 monthly income? That’s not affordable-it’s a trap.
Parent advocacy groups like Families USA found that 42% of families who went through a coverage transition blamed bureaucratic delays tied to substitution rules. They waited weeks for answers. Kids missed doctor visits. Vaccines got delayed. One mother in Texas told a NASHP focus group: “I had to choose between paying rent and buying my son’s asthma inhaler because CHIP wouldn’t approve him until the waiting period was over.”
But there’s another side. Texas CHIP administrators argue that without waiting periods, employers might drop coverage entirely, knowing the state will pick up the tab. They say substitution rules keep private insurance intact. And data backs that up: since 2010, substitution rules have prevented an estimated $1.3 billion in inappropriate CHIP spending each year, according to MACPAC.
The real problem? The rules were designed in the 1990s. Back then, jobs were more stable. Insurance didn’t change every few months. Now, gig work, seasonal labor, and short-term plans are common. A 90-day waiting period doesn’t make sense when someone can lose coverage on a Friday and need help Monday.
What’s Changing in 2025 and Beyond
The 2024 CMS rule is the biggest update in over a decade. States now have to:
- Share data automatically between Medicaid and CHIP
- Accept eligibility decisions from other programs (like ACA marketplace plans)
- Report quarterly on coverage gaps and waiting period use
By October 1, 2025, all states must have the tech in place to make these changes. By December 31, 2025, they must start accepting eligibility determinations from other insurance programs. That means if a family gets denied a marketplace plan because they’re too poor, Medicaid can step in faster.
Experts predict that by 2027, every state will use automated data matching. Manatt Health forecasts a 65% drop in manual verification. That’s good news. But the Urban Institute warns: if no further updates happen, substitution rules could become 25% less effective by 2030. The insurance market keeps changing. The rules haven’t kept up.

What Families Should Know
If you’re applying for Medicaid or CHIP and you have access to private insurance, don’t assume you’re automatically denied. Ask:
- Is the premium more than 9.12% of my household income?
- Is the coverage actually active and being used?
- Do I qualify for an exemption because of job loss, reduced hours, or a recent move?
Some states make it easy to apply for exemptions. Others don’t. If you’re denied and think it’s wrong, appeal. Call your state’s Medicaid office. Ask for the substitution policy document. Most states have one online.
And if you’re a parent in a state with a 90-day waiting period-don’t wait. Apply for CHIP anyway. Even if you’re denied, you’ve started the process. You might get approved sooner than you think.
Frequently Asked Questions
Are Medicaid substitution rules the same in every state?
No. While all states must follow federal rules to prevent Medicaid or CHIP from replacing affordable private insurance, how they do it varies. Thirty-four states use a waiting period of up to 90 days, while 16 states rely on real-time data checks instead. Some states add extra exemptions for job loss or seasonal work, others don’t. The core requirement is the same, but the methods are not.
Can a child be denied CHIP just because a parent has job-based insurance?
Only if that insurance is considered affordable-meaning the employee’s share of the premium doesn’t exceed 9.12% of household income in 2024. If the cost is too high, the child can still qualify for CHIP. States must verify affordability, not just the existence of coverage.
What happens if a family loses their private insurance and needs CHIP right away?
Federal law requires states to waive waiting periods if a family loses job-based coverage. States must allow immediate enrollment in CHIP in cases of job loss, reduced hours, or divorce. But in practice, some states still delay. If you’re denied, file an appeal and ask for the exemption form.
Why do some states use waiting periods and others don’t?
States that use waiting periods say it prevents employers from dropping coverage, saving public money. States that avoid them say the rules create coverage gaps and hurt working families. States with better data systems-like Minnesota and Oregon-don’t need waiting periods because they can verify coverage in real time. Those still using paper forms rely on waiting periods because they lack the tech to check faster.
Is the 90-day waiting period still fair in today’s economy?
Many experts say no. The rule was written in the 1990s, when jobs were more stable. Today, gig work, seasonal labor, and frequent job changes are common. A 90-day wait can leave kids without care during a medical emergency. The 2024 CMS rule is moving toward faster transitions, but full modernization is still underway.
How can I find out my state’s substitution rules?
Visit your state’s Medicaid or CHIP website and search for “substitution policy” or “CHIP eligibility.” Most states publish their rules online. You can also call the state’s Medicaid helpline and ask for the written policy under 42 CFR 457.805. If the information is unclear, ask for a copy of their internal staff guidance-frontline workers often have better access to the real process.
What Comes Next
If you’re a parent, keep applying-even if you’re turned down. Document every denial. Ask for the reason in writing. If your child goes without care, contact your local health advocate group. They can help you navigate appeals.
If you’re a state worker, push for better data systems. The 2024 rule gives you funding and deadlines to upgrade. Use them. The families you serve don’t care about policy debates-they care about whether their kid can see a doctor next week.
The system isn’t broken because of bad intentions. It’s broken because it’s outdated. The fix isn’t more rules. It’s faster tech, smarter data, and less waiting. That’s what the next five years will be about-and it’s already starting.

It’s frustrating how often families get caught in the gap between systems. I’ve seen parents work two jobs just to stay above the income threshold, only to be denied CHIP because ‘they had access’-but access doesn’t mean they could actually afford it. The 9.12% rule sounds fair on paper, but when rent is $1,800 and groceries are $600, that premium becomes a luxury. We need to stop pretending this is about policy and start treating it like a human crisis.
Honestly, I didn’t realize how much variation there was between states. My cousin in Texas got denied for 90 days even though her husband lost his job the week before. Meanwhile, my sister in Minnesota got automatic enrollment because their systems talk to each other. Why are we still using paper forms in 2025? It’s not about saving money-it’s about laziness disguised as policy.
There’s a quiet moral contradiction here. We say we value family, yet we design systems that force parents to choose between paying rent and filling prescriptions. The substitution rules were meant to protect private insurance, but they’ve become a proxy for punishing poverty. The real question isn’t whether Medicaid should replace coverage-it’s whether we’re willing to admit that ‘affordable’ is a myth for millions of working families. Maybe the fix isn’t better tech-it’s better empathy.
Let me be unequivocally clear: the current framework is a bureaucratic abomination masquerading as fiscal prudence. The 90-day waiting period is not merely archaic-it is a grotesque, systemic failure that violates the most basic tenets of public health ethics. States clinging to antiquated paper-based verification protocols are not merely inefficient-they are complicit in the preventable suffering of children. The 2024 CMS rule is a necessary corrective, but without mandatory federal funding for interoperable data infrastructure, we are merely rearranging deck chairs on the Titanic. The time for incrementalism is over; we require revolutionary integration or we must dismantle the entire architecture.
The federal government has NO BUSINESS forcing states to change their rules! This is a STATE issue! If Texas wants to use a 90-day waiting period to protect private insurance markets, that’s their RIGHT! You liberals want to turn Medicaid into a free-for-all, but that’s just socialism! And don’t get me started on ‘gig workers’-if you can’t hold a real job, you shouldn’t get government help! The system works fine if people just took responsibility! End of story!
Utterly predictable. The American welfare state continues its descent into performative chaos. The 90-day waiting period is a rational, time-tested mechanism to prevent moral hazard. The real issue? The proliferation of part-time, gig-based employment-a symptom of cultural decay, not policy failure. Europe, by contrast, maintains orderly, means-tested systems without such theatrical inefficiencies.
bro i live in india and we dont even have this kind of system, but i read this and i feel bad for the families. in usa you have so much tech but still people wait months for a kid to get medicine? that dont make sense. maybe you need to just let people apply and check later? like in india we do aadhaar and then verify, not the other way. also why paper forms? why not just use the tax data? its all there. i dont get it.
The 2024 CMS rule represents a significant step toward operational coherence. However, its efficacy remains contingent upon state-level implementation fidelity. Data interoperability, while technically feasible, requires sustained investment and institutional buy-in. The persistent reliance on manual verification in 22 states suggests structural inertia rather than technical limitation. A longitudinal study comparing pre- and post-rule coverage gaps would yield valuable policy insights. Until then, anecdotal evidence-however compelling-remains insufficient to justify systemic overhaul.