NMS Symptom Checker
This tool helps identify key symptoms of Neuroleptic Malignant Syndrome (NMS), a rare but life-threatening reaction to dopamine-blocking medications. Important: This is not a diagnostic tool. If you or someone you know has these symptoms, seek immediate medical attention.
Four Key Symptoms to Watch For
NMS requires all four of these symptoms for diagnosis, though they don't always occur simultaneously. Missing even one symptom can delay critical treatment.
Neuroleptic Malignant Syndrome (NMS) isn’t something most people hear about until it’s too late. It doesn’t show up in TV medical dramas as a dramatic twist-it shows up in hospital ICUs, often mistaken for a worsening psychiatric episode or a bad infection. And when it’s missed, the consequences can be fatal. This isn’t just a rare side effect. It’s a medical emergency that demands immediate recognition and action.
What Exactly Is Neuroleptic Malignant Syndrome?
NMS is a life-threatening reaction to medications that block dopamine in the brain. These include older antipsychotics like haloperidol and chlorpromazine, but also newer ones like risperidone and olanzapine. Even some anti-nausea drugs-metoclopramide and promethazine-can trigger it. The core problem? Dopamine stops working properly in two key areas: the part of the brain that controls movement, and the part that regulates body temperature.
When dopamine receptors get blocked, muscles lock up, the body can’t cool itself, and the nervous system goes haywire. The result? A deadly mix of symptoms that usually show up within the first two weeks of starting or increasing a medication, though they can appear as early as 48 hours or as late as months later.
The Four Signs You Can’t Ignore
Doctors look for four things when they suspect NMS. Missing even one can delay diagnosis. Here’s what to watch for:
- Severe muscle rigidity-not just stiffness, but a deep, unyielding tightness called "lead pipe" rigidity. If you try to move someone’s arm, it feels like bending a steel pipe-no give, no resistance, just constant tension.
- High fever-temperature over 100.4°F (38°C), often climbing past 104°F (40°C). This isn’t a typical fever from infection. It’s the body overheating from muscles working nonstop.
- Altered mental state-confusion, agitation, delirium, or worse, complete mutism and unresponsiveness. Patients can’t speak, can’t move, and seem detached from reality.
- Autonomic instability-wild swings in heart rate (over 90 bpm), blood pressure (spiking or crashing), sweating, and rapid breathing. This is the body’s automatic systems losing control.
These symptoms don’t all hit at once. Usually, mental changes come first, then muscle rigidity, then fever, and finally the chaotic vital signs. But in real life, they often overlap. That’s why so many cases are missed.
Why NMS Gets Misdiagnosed
One of the biggest dangers with NMS is that it looks like something else. In fact, up to 12% of cases are initially labeled as a psychiatric flare-up. A patient on risperidone who suddenly becomes unresponsive? Doctors might think their schizophrenia is getting worse. A person on metoclopramide with a fever and stiff muscles? Maybe it’s the flu.
But the clues are there. NMS doesn’t cause cough, runny nose, or sore throat. It doesn’t respond to antibiotics. And unlike serotonin syndrome-which also causes fever and confusion-NMS doesn’t have clonus (involuntary muscle jerks) or diarrhea. It has lead pipe rigidity, not twitching.
Even in emergency rooms, only about 60% of doctors correctly identify NMS on first glance, according to a 2021 study. That’s why patient stories often include phrases like: “It took two days for them to realize it wasn’t just my mind playing tricks.”
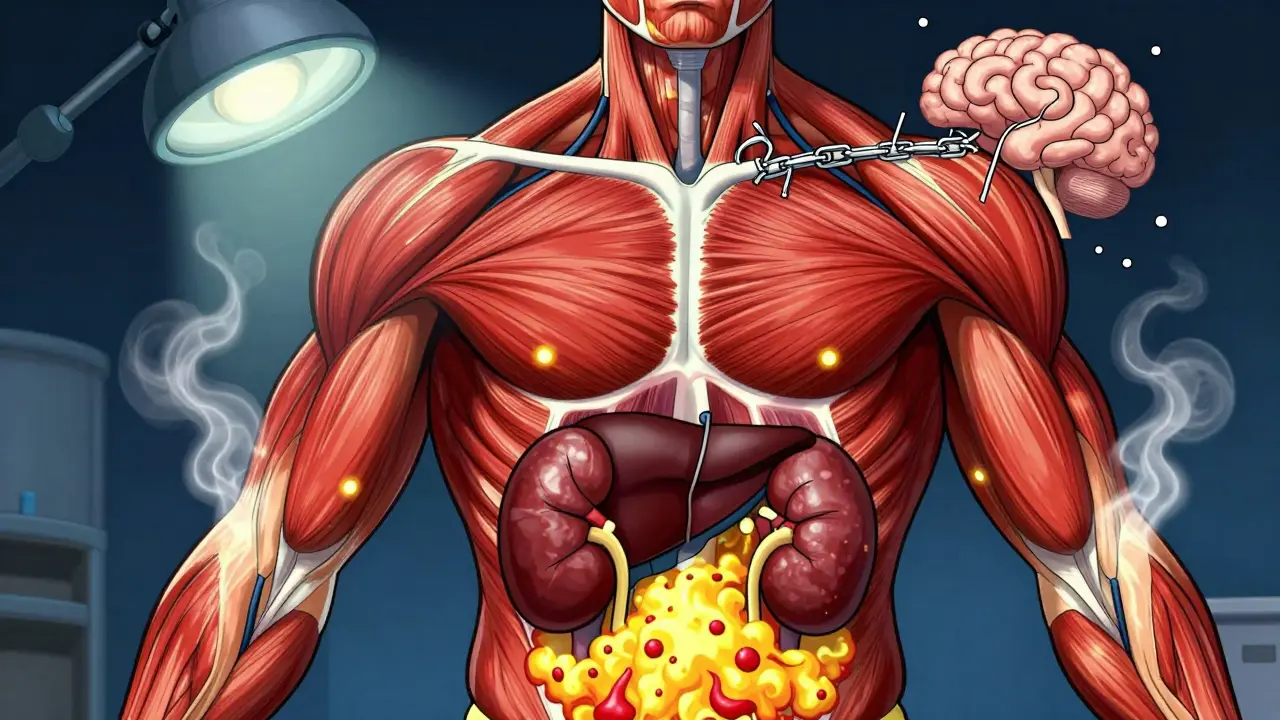
What Happens in the Body?
Beneath the symptoms, something dangerous is happening inside. The muscles are locked in constant contraction, burning through energy and releasing a toxic protein called myoglobin into the bloodstream. That’s why creatine kinase (CK) levels skyrocket-sometimes over 100,000 IU/L (normal is under 200). This isn’t just muscle soreness. It’s muscle breakdown on a massive scale.
Myoglobin floods the kidneys, causing acute kidney injury in about 30% of cases. The liver can also get damaged, with liver enzymes spiking. Blood potassium rises dangerously high. White blood cell counts climb, mimicking infection. Iron levels drop. All of this adds up to multi-organ stress.
And here’s the scary part: even if the fever breaks and the muscles relax, the damage can linger. One patient on a schizophrenia support forum said it took eight weeks before they could walk without help. Muscle weakness doesn’t always vanish after recovery.
Who’s at Risk?
NMS isn’t random. Certain factors make it more likely:
- Starting or increasing a high-potency antipsychotic (like haloperidol) too quickly-especially by more than 5 mg per day
- Using injectable forms of antipsychotics
- Combining antipsychotics with lithium or other dopamine-altering drugs
- Being male and under 40
- Having bipolar disorder instead of schizophrenia
- Having Parkinson’s disease and suddenly stopping dopaminergic meds
Most cases happen when someone is first put on an antipsychotic (60%), or when their dose is raised (30%). Only 10% occur in people who’ve been stable on the same dose for months or years.
How Is It Treated?
There’s no magic pill. Treatment is fast, aggressive, and focused on stopping the damage before it’s irreversible.
- Stop the drug immediately. No exceptions. All dopamine-blocking medications must be discontinued-antipsychotics, anti-nausea drugs, even certain antivert medications.
- Cool the body. If the temperature is above 102°F (38.9°C), use cooling blankets, fans, and ice packs. IV fluids help lower core temperature and protect the kidneys.
- Hydrate aggressively. At least 1-2 liters of IV fluids upfront, then 100-150 mL per hour to keep urine flowing. Goal: at least 30 mL per hour to flush out myoglobin.
- Use specific medications. Dantrolene (given IV) helps relax muscles and reduce heat production. Bromocriptine or apomorphine (still experimental) can restart dopamine signaling. Dantrolene is used in about 70% of cases, and studies show it cuts recovery time by days.
- Monitor in the ICU. Continuous heart, kidney, and temperature monitoring is non-negotiable. CK levels are checked every 6-12 hours until they peak (usually 72-96 hours after onset).
Some patients need dialysis. Some need breathing support. Recovery usually takes 7 to 10 days if caught early. But if treatment is delayed beyond 24 hours, the risk of permanent damage or death jumps dramatically.
Survival Rates Are Better Now-But Not Perfect
Twenty years ago, NMS killed 20% of patients. Today, with better awareness and protocols, that number has dropped to around 5%. That’s progress. But 5% is still 1 in 20 people. And for those who survive, 15% still have muscle weakness at 30 days.
Second-generation antipsychotics like quetiapine and clozapine have made NMS far rarer-down to 0.01% to 0.02% of users, compared to 0.5% to 2% with older drugs. But they’re not risk-free. The FDA added a black box warning to all antipsychotics in January 2023, noting that 12% of NMS cases happen even at therapeutic doses in people with no known risk factors.
What Happens After Recovery?
Survivors often face a hard choice: go back on antipsychotics or risk a relapse of psychosis or mania. A 2022 survey found that 65% of NMS survivors were afraid to restart these medications-even when their mental health demanded it.
Reintroducing antipsychotics after NMS is possible, but it’s done cautiously: waiting at least two weeks, starting with a very low dose of a low-risk drug (like clozapine or quetiapine), and monitoring closely. Some doctors avoid all dopamine blockers after NMS, even if it means using non-standard treatments.
There’s no one-size-fits-all answer. But ignoring the fear isn’t the answer either. Patients need support, clear communication, and a team that understands both the psychiatric and neurological risks.
What’s Next for NMS?
Researchers are working on faster ways to catch NMS before it escalates. Some hospitals are testing AI tools that scan electronic records for early signs-like a sudden spike in CK, fever, and muscle rigidity-and flag potential cases 24 hours before a doctor would notice. Early results show 85% accuracy.
There’s also a clinical trial underway testing intranasal apomorphine, a dopamine agonist that can be sprayed into the nose. In early tests, it brought down fever in 70% of patients within 4 hours-compared to 12 hours with standard care. If it works, it could become a game-changer.
For now, the best defense is awareness. If you’re on an antipsychotic-or caring for someone who is-and they suddenly develop stiffness, fever, confusion, or rapid heartbeat, don’t wait. Don’t assume it’s just their illness getting worse. Call for emergency help. Say the words: “Could this be NMS?”
It’s rare. But when it happens, speed saves lives.


NMS isn't a side effect. It's a system failure. Dopamine isn't just a neurotransmitter-it's the governor of movement, temperature, and awareness. Block it, and the body reverts to primal chaos. No drama. No warning. Just silence before the storm.
They don't want you to know this is all part of the pharmaceutical control agenda. Antipsychotics? Designed to make you docile. NMS? A cover-up for the side effects they knew about since the 70s. The FDA’s black box warning? A PR stunt. They’re still selling these drugs like candy. Wake up.
i saw this happen to my cousin after they gave her that anti-nausea shot at the ER… she just locked up and stared at the ceiling for hours. nobody believed us until her temp hit 105. now i check every med label like a hawk. 🤢
thank you for writing this with such care 💛 i’ve watched someone i love go through this and the silence around it was heavier than the rigidity itself. people don’t talk about how scary it is to be trapped in your own body while everyone thinks you’re ‘acting out’… but you’re not. you’re screaming inside. this post matters.
This is an exceptionally well-researched and clinically accurate overview. The emphasis on early recognition and immediate discontinuation of causative agents is paramount. I would only add that interdisciplinary collaboration between psychiatry, neurology, and critical care teams significantly improves outcomes. Education must be institutionalized, not left to chance.
I’ve been a nurse for 22 years, and I still get chills thinking about the first NMS case I saw… the way the muscles just… froze… like a statue made of pain. We didn’t have dantrolene back then. We just held their hands and prayed. Please, if you’re a provider-don’t wait for all four signs. One is enough to start sounding alarms.
One must interrogate the ontological framework of pharmacological hegemony. The dopamine hypothesis, itself a reductive metaphysical construct, pathologizes subjective experience under the guise of neurochemical equilibrium. NMS, then, is not merely iatrogenic-it is the corporeal manifestation of epistemic violence perpetrated by the biomedical apparatus upon the phenomenological subject. The body, in its refusal, becomes the last site of resistance.
Everyone talks about NMS like it's some big mystery but it's not. People just don't take care of themselves. If you're on these drugs, you should be eating right, sleeping, not mixing with alcohol or weed. I knew a guy who took haloperidol and drank energy drinks every day-he got NMS and then acted surprised. No, buddy, you did this to yourself. It's not the drug's fault, it's your lifestyle. Simple.
Why are we letting Big Pharma push these drugs on our kids? In America, we’re medicating normal behavior. NMS is just the tip of the iceberg. We need to stop this. No more pills for sadness. No more pills for being different. We used to handle mental health with discipline, not chemistry. Our country’s getting weaker.
For anyone reading this who’s scared to restart meds after NMS-you’re not alone. I survived it, and I did go back on clozapine, slowly, with a team watching me like a hawk. It’s terrifying, but it’s possible. You deserve to feel like yourself again. Just don’t do it alone. Find your people. I’m here if you need to talk.
The real tragedy isn’t NMS-it’s that we treat psychiatric illness as something to be suppressed, not understood. We lock dopamine in a cage and expect the body not to rebel. But the mind isn’t a machine. You can’t fix a soul with chemistry and call it progress. NMS is the body’s protest. We should listen.