When you're on clopidogrel after a heart attack or stent placement, your doctor isn't just thinking about your heart-they're thinking about your stomach too. Many people on clopidogrel also need a proton pump inhibitor (PPI) like omeprazole to prevent ulcers. But here's the catch: omeprazole can seriously weaken clopidogrel’s ability to protect your heart. This isn’t a theoretical concern. It’s a well-documented, clinically significant interaction that affects how well your blood thins-and whether you’re at risk for another heart event.
How Clopidogrel Actually Works (It’s Not What You Think)
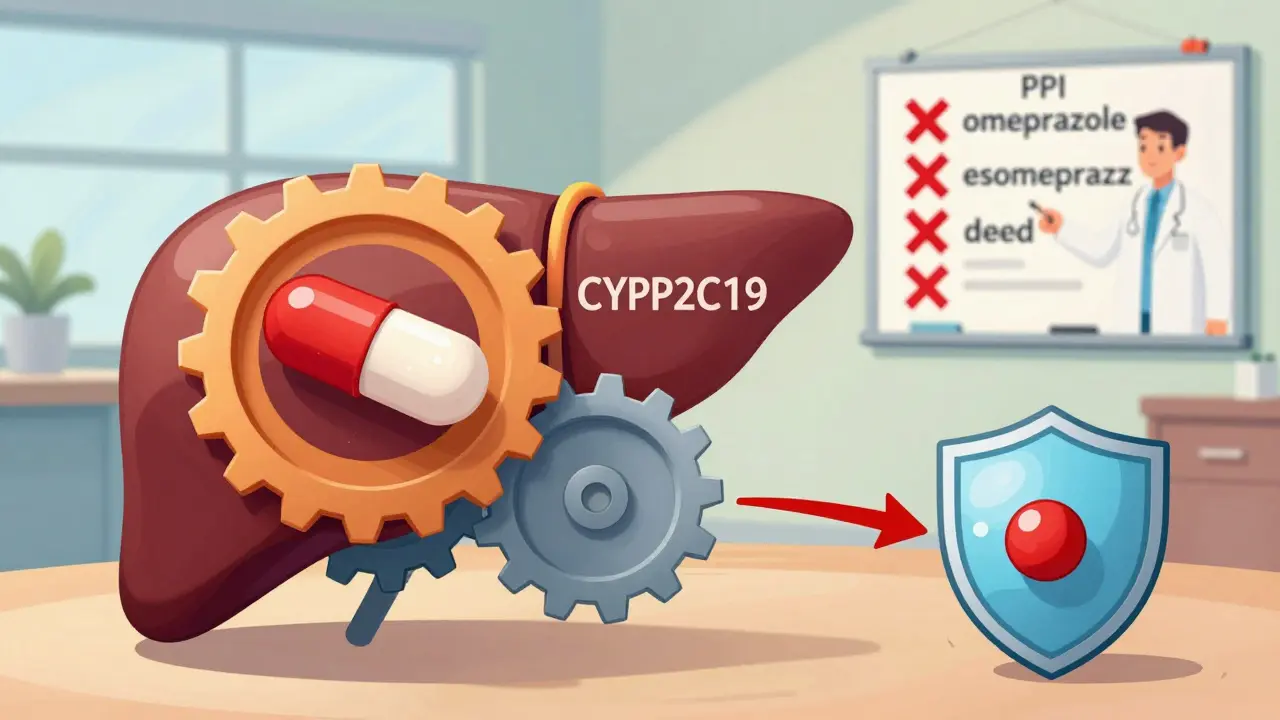
Clopidogrel doesn’t work by itself. It’s a prodrug, meaning your body has to turn it into something active before it does anything. That active form blocks a receptor on platelets called P2Y12, which stops them from clumping together and forming dangerous clots. But getting there isn’t simple. Two steps in your liver are needed, and both rely heavily on one enzyme: CYP2C19. If that enzyme is blocked, clopidogrel can’t activate. And that’s exactly what omeprazole does.Why Omeprazole Is the Problem
Omeprazole is one of the most commonly prescribed PPIs for acid reflux and ulcers. It works by reducing stomach acid, which is great for your stomach. But it also binds tightly to CYP2C19-the same enzyme clopidogrel needs. Studies show that even a standard 20mg daily dose of omeprazole can reduce clopidogrel’s active metabolite by 32%. At 80mg, that number jumps to 49%. That’s not a small drop. That’s enough to make clopidogrel less effective at preventing clots.The FDA issued a safety warning in 2009 after multiple studies confirmed this. One study by Brandt et al. found that omeprazole 80mg cut clopidogrel’s active metabolite exposure by 45%. Another, by Sibbing et al., showed patients taking both drugs had higher rates of stent thrombosis-when a clot forms inside the stent, which can cause a heart attack.
Not All PPIs Are Created Equal
This isn’t a blanket warning against all PPIs. The problem is specific to omeprazole-and its close cousin, esomeprazole (the S-isomer of omeprazole). Other PPIs have much weaker effects on CYP2C19.- Omeprazole: Strong inhibitor. IC₅₀ of 2-4 μM. Reduces clopidogrel’s active metabolite by up to 49% at high doses.
- Esomeprazole: Nearly as bad. At 40mg daily, it cuts active metabolite levels by 40%.
- Lansoprazole: Mild effect. Standard 30mg dose reduces clopidogrel exposure by only 5%. High doses (60mg) may lower peak levels by 18%.
- Pantoprazole: Minimal interaction. At 40mg daily, it reduces exposure by just 14%. This is the most recommended alternative.
- Rabeprazole: Low impact. Reduces peak levels by 28% but doesn’t affect overall exposure significantly.
- Ilaprazole: Weakest inhibition. Recent 2025 data shows no clinically relevant effect on clopidogrel.
These differences aren’t just numbers on a page. They directly impact your risk. If you’re on clopidogrel and need a PPI, pantoprazole is the safest pick. Rabeprazole is a decent second choice. Omeprazole and esomeprazole should be avoided.
The Genetic Factor: Your DNA Matters
Not everyone reacts the same way. About 30% of people of East Asian descent-and 20-25% of Caucasians-carry a genetic variant called CYP2C19*2 or *3. These are loss-of-function alleles. If you have one or two of them, your body naturally produces less of the enzyme that activates clopidogrel. Add omeprazole into the mix, and your clopidogrel becomes almost useless.A 2012 Korean study found that in people with normal CYP2C19 function, omeprazole reduced clopidogrel’s effect by 32%. In those with intermediate metabolism, it dropped by 54%. That’s not a small risk. That’s a major safety issue. The Clinical Pharmacogenetics Implementation Consortium (CPIC) now recommends testing for these variants if you’re on clopidogrel and need a PPI. If you’re a poor metabolizer, switch to prasugrel or ticagrelor-two newer antiplatelet drugs that don’t rely on CYP2C19.
What the Studies Really Say
There’s a lot of noise out there. Some studies say the interaction doesn’t matter. Others say it’s life-threatening. Why the contradiction?The COGENT trial (2010) looked at 3,761 patients and found no increase in heart attacks or strokes when omeprazole was taken with clopidogrel. But that trial used only 10mg of omeprazole-less than the dose shown to cause the biggest interaction. Also, most patients were low-risk.
On the other side, a meta-analysis of 271,551 patients found that PPI use raised the risk of cardiovascular events by 27%. Omeprazole alone increased risk by 33%. The FAST-MI Registry, which tracked 2,744 patients, found no increased risk. But two-thirds of those patients were on omeprazole.
The truth? The interaction is real in the lab and in pharmacokinetic studies. But whether it leads to more heart attacks depends on your risk level, your genetics, your dose, and your overall health. High-risk patients-those with stents, recent heart attacks, or diabetes-are the ones most vulnerable.

What Should You Do?
If you’re on clopidogrel and need a stomach medication, here’s what to do:- Avoid omeprazole and esomeprazole. They’re the biggest offenders.
- Choose pantoprazole. It’s the most studied and safest PPI option with clopidogrel.
- Consider rabeprazole if pantoprazole isn’t available. It’s a good alternative.
- Ask about H2 blockers. Famotidine (Pepcid) doesn’t affect CYP2C19 and can be used for short-term acid control.
- Ask about genetic testing. If you’re at high risk for clotting or have a family history of heart problems, CYP2C19 testing can guide your treatment.
- Don’t split doses. Taking clopidogrel in the morning and omeprazole at night doesn’t help. The inhibition is systemic, not timing-dependent.
The American College of Gastroenterology and the American Heart Association both recommend pantoprazole as first-line for patients on clopidogrel who need acid suppression. The European Society of Cardiology says to avoid omeprazole and esomeprazole entirely.
The Bigger Picture
Since the FDA warning in 2009, prescriptions for omeprazole with clopidogrel dropped by 65% in the U.S. Meanwhile, pantoprazole use rose by 42%. That’s not just doctors changing their minds-it’s evidence driving practice. The market for antiplatelet drugs is worth over $13 billion, and the clopidogrel-PPI issue helped push the adoption of newer agents like ticagrelor and prasugrel, which aren’t affected by CYP2C19 inhibitors.Now, research is moving toward even smarter solutions. Ilaprazole, a newer PPI, shows almost no inhibition of CYP2C19 in 2025 studies. Three new antiplatelet drugs in Phase II trials are being designed to bypass CYP2C19 entirely. Personalized medicine isn’t the future-it’s here. If you’re on clopidogrel, your doctor should be asking: Do you need a PPI? And if so, which one?
Final Takeaway
This isn’t about avoiding all PPIs. It’s about choosing the right one. Omeprazole and clopidogrel together can be dangerous-not because they’re toxic, but because they cancel each other out. Your heart needs clopidogrel to work. Your stomach needs acid control. You don’t have to choose between them. You just need the right combination.If you’re on clopidogrel and taking omeprazole, talk to your doctor. Don’t stop either drug on your own. But do ask: Is there a safer option? The answer might be simpler than you think.
Can I take omeprazole with clopidogrel if I take them at different times of day?
No. Timing doesn’t matter. Omeprazole inhibits the CYP2C19 enzyme in your liver, not in your stomach. Whether you take clopidogrel in the morning and omeprazole at night, the enzyme is still blocked. The interaction is systemic and continuous, not affected by dosing schedule.
Is pantoprazole completely safe with clopidogrel?
Pantoprazole has the weakest interaction with CYP2C19 among commonly used PPIs. Studies show it reduces clopidogrel’s active metabolite by only about 14%, which is not considered clinically significant. Major guidelines, including those from the American College of Gastroenterology, recommend pantoprazole as the preferred PPI when used with clopidogrel.
What if I’m already on omeprazole and clopidogrel-should I stop one?
Do not stop either medication without talking to your doctor. Stopping clopidogrel suddenly increases your risk of heart attack or stroke. Stopping omeprazole could cause serious stomach damage if you’re at risk for ulcers. Instead, ask your doctor to switch you to pantoprazole or rabeprazole. That’s a safer, manageable change.
Are there other drugs besides omeprazole that interfere with clopidogrel?
Yes. Fluconazole, fluoxetine, citalopram, and some antifungals and antidepressants also inhibit CYP2C19. Even over-the-counter medications like St. John’s Wort can affect it. Always tell your doctor or pharmacist about all medications and supplements you’re taking-prescription, OTC, or herbal.
Why do some studies say the interaction doesn’t matter?
Some studies, like the COGENT trial, didn’t find increased heart events because they used low-dose omeprazole (10mg) and included mostly low-risk patients. Other studies, like the meta-analysis of 271,000 patients, found clear risk because they included higher-risk populations and higher doses. The interaction is real in pharmacokinetics. Whether it leads to more heart attacks depends on your individual risk profile, genetics, and dose.
Can I use famotidine instead of a PPI with clopidogrel?
Yes. Famotidine (Pepcid) is an H2 blocker, not a PPI. It doesn’t affect CYP2C19 and is a safe alternative for short-term acid control. However, it’s less effective than PPIs for long-term ulcer prevention or severe GERD. Use it only if you need temporary relief or if your doctor recommends it as a bridge while switching PPIs.
Should I get tested for CYP2C19 if I’m on clopidogrel?
If you’re at high risk for clotting (e.g., after a stent, heart attack, or stroke) and you need a PPI, yes. About 30% of people in East Asian populations and 20-25% in Caucasian populations carry loss-of-function variants. If you’re one of them, clopidogrel may not work well-even without omeprazole. Testing can help your doctor choose a better drug, like ticagrelor or prasugrel, which don’t rely on CYP2C19.

Wow. So omeprazole is basically the villain in this superhero movie and pantoprazole is the quiet sidekick who saves the day? I’ve been on both and honestly? I didn’t even know this was a thing. My cardiologist just said ‘take the red pill’ and I did. Now I feel like I’ve been betrayed by my stomach meds. 😅
Thank you for this meticulously researched and profoundly important summary. The distinction between pharmacokinetic interaction and clinical outcome is often lost in public discourse. This post bridges that gap with clarity and compassion.
As a clinical pharmacist, I have repeatedly counseled patients on this exact issue. The data is unequivocal. Omeprazole and esomeprazole must be avoided in patients on clopidogrel. Pantoprazole remains the gold standard. This is not a matter of opinion-it is standard of care.
so like... i just found out i been takin omeprazole with my clopidogrel for 2 years?? like wtf?? my doc never said nothin and now im scared to even look at my pill bottle??
Studies show interaction. But real world data? Mixed. Stop overreacting. Your body is not a test tube. Many live fine on both. Stop fearmongering.
Of course the FDA warned about this in 2009. But you know who still prescribes omeprazole? Doctors who don't read journals. They're lazy. They don't care about your heart. They care about their next coffee break. And you? You're just a number on their screen.
Okay but let’s be real-this whole thing is why big pharma pushed ticagrelor and prasugrel so hard. Omeprazole was the perfect scapegoat. If you’re a high-risk patient, just switch to the newer drugs. No PPI drama. No genetic testing. Just pay $400 a month and call it a day. Profit over physiology, always.
Let me just say-this isn’t about CYP2C19. This is about the slow, creeping erosion of medical autonomy. The guidelines? Written by committees with ties to PPI manufacturers. The ‘safety warning’? A marketing maneuver disguised as science. You think you’re being protected? You’re being herded. Into a more expensive, less natural solution. Wake up.
People are dying because doctors won't stop prescribing omeprazole. I had a friend who had a stent and was on omeprazole for ‘heartburn’-turns out he had silent ischemia and the clopidogrel wasn't working. He ended up in the ICU. This isn't a ‘maybe’-it's a silent killer and nobody talks about it
Interesting. I’ve been on pantoprazole for years with clopidogrel. Never had an issue. But I never knew why. Good to see the science laid out clearly. Thanks for the clarity.
Bro this is wild. I just switched from omeprazole to pantoprazole last month because my stomach was acting up. Didn’t know I was saving my heart too. Mind blown. Thanks for the heads up!
Ilaprazole? 2025 data? That’s not even approved yet. Why are you citing unpublished studies? This reads like a blog post masquerading as clinical guidance.
As someone from India, I see this all the time. Omeprazole is cheap, available everywhere, and doctors just prescribe it. No testing, no alternatives. We need better education. Maybe this post can help. Thank you for writing this.
Here’s the truth they don’t want you to know: CYP2C19 isn’t the real issue. The real problem is that your gut microbiome is being destroyed by PPIs, which then alters how your liver metabolizes everything-including clopidogrel. The FDA warning? A distraction. The real villain is industrial medicine. They want you dependent. On pills. On tests. On fear. They don’t want you healing naturally. This is all a controlled narrative. Ask yourself: Who profits from your confusion?