Snoring isn’t just annoying-it’s a sign your airway is collapsing while you sleep. If you’ve tried pillows, nasal strips, or sleeping on your side and still hear that loud rumble night after night, you’re not alone. Over 34 million American adults snore habitually, and for many, the problem doesn’t go away with lifestyle changes. That’s where oral appliance therapy comes in. Specifically, mandibular advancement devices (MADs) offer a proven, non-invasive way to reduce or even eliminate snoring by gently moving your lower jaw forward. Unlike CPAP machines, they’re quiet, portable, and don’t require a mask. But are they right for you? And what’s the real cost-both financially and physically?
How Mandibular Advancement Devices Actually Work
Mandibular advancement devices look like sports mouthguards, but they’re precision medical tools. They work by holding your lower jaw slightly forward-usually between 3 and 10 millimeters-while you sleep. This small movement pulls your tongue and soft tissues away from the back of your throat, keeping your airway open. No collapsing airway means no snoring.
The science behind this isn’t new. Back in 1999, Dr. Nobuyoshi Kato showed that every extra millimeter of jaw advancement reduced breathing interruptions. Today, we know that the sweet spot for most people is around 75% of their maximum possible jaw protrusion, which typically translates to 8-10mm. Too little, and it won’t help. Too much, and you risk jaw pain or dental damage.
Custom-made MADs are built from semi-rigid acrylic with titanium connectors, molded precisely to your teeth. Over-the-counter versions use thermoplastic that you soften in hot water and bite into. But here’s the catch: custom devices work significantly better. A 2015 meta-analysis found custom MADs reduced snoring by 72.3% on average, while store-bought ones only hit 48.6%. The difference isn’t just in comfort-it’s in effectiveness.
Who Benefits Most from Oral Appliance Therapy
Not everyone who snores is a good candidate. MADs work best for people with mild to moderate obstructive sleep apnea-or those with primary snoring (snoring without apnea). If your snoring is loud, frequent, and accompanied by gasping or daytime fatigue, you should get a sleep study first. Severe sleep apnea still needs CPAP.
You’re also a good fit if you:
- Have at least 6-8 natural teeth in both upper and lower jaws
- Don’t have active gum disease or loose teeth
- Have healthy temporomandibular joints (TMJ)-no clicking, pain, or locking
- Prefer a quiet, portable solution over a bulky machine
People with Mallampati Class IV airways (very limited throat visibility) or those who collapse completely during sleep often don’t respond. Studies show failure rates hit 38.6% in these cases. If you’ve tried CPAP and hated it-because of the mask, noise, or claustrophobia-MADs are often the next best option.
How Effective Are They Compared to Other Treatments
Let’s cut through the hype. MADs don’t cure snoring for everyone, but they work better than most over-the-counter fixes.
Here’s how they stack up:
| Treatment | Snoring Reduction | Adherence Rate (12 Months) |
|---|---|---|
| CPAP | 85-95% | 45.2% |
| Custom MAD | 65-75% | 76.4% |
| OTC MAD | 30-50% | 61% |
| Positional Therapy | 35-45% | 58% |
| Nasal Dilators | 20-30% | 42% |
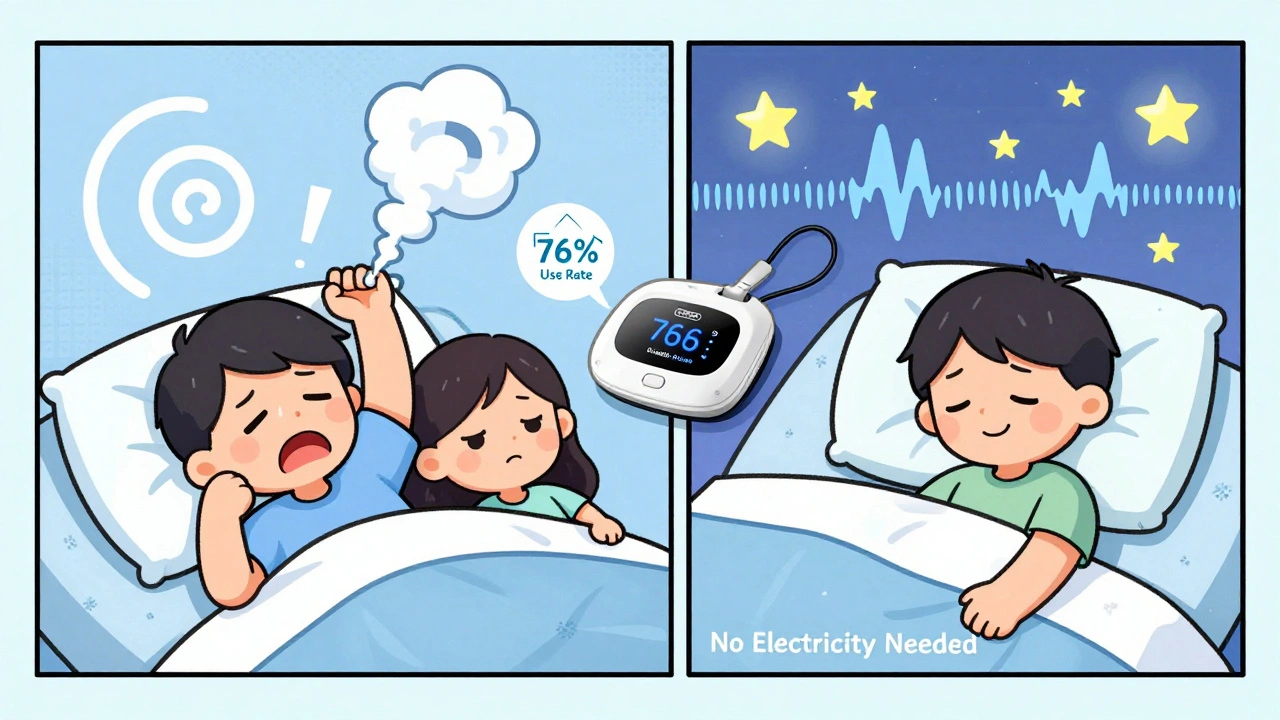
CPAP is more effective at stopping snoring entirely-but most people quit using it. MAD users stick with it longer. In fact, the SAVE trial showed 76.4% of MAD users were still using theirs after a year, compared to just 45.2% for CPAP. That’s why the American Academy of Sleep Medicine recommends MADs as a first-line treatment for mild-to-moderate sleep apnea and primary snoring.
They’re also great for travel. No electricity. No hose. Just pop it in your case and go. If you’re a frequent flyer or camper, this matters.

The Real Cost: Money, Time, and Dental Risks
Custom MADs cost between $1,800 and $2,500. Insurance rarely covers them-only 38% of U.S. plans do, according to 2023 data. That’s a big hurdle. But consider this: if you’ve spent $200 a year on nasal strips, pillows, and sprays for five years, you’re already at $1,000. A custom device lasts 3-5 years with proper care.
There’s also the time cost. Getting a custom MAD isn’t quick. You need:
- A sleep study (to rule out severe apnea)
- A dental exam (to check your teeth and jaw)
- Dental impressions or a 3D scan
- 2-3 follow-up visits over 4-6 weeks to adjust the device
Each visit costs $150-$300. Total out-of-pocket? $2,500-$3,500 if uninsured.
And then there’s the dental risk. About 25% of long-term users develop permanent changes in their bite. Teeth can shift. The jaw joint can become sore. Some people need braces or crowns years later. Dr. Avram Gold from SUNY warns that these changes are often irreversible. That’s why regular dental check-ups every 6 months are non-negotiable.
What to Expect in the First Few Weeks
Most people don’t love their MAD at first. Here’s what’s normal:
- Morning jaw pain-68% of users report this in the first week. It usually fades in 2-4 weeks.
- Excessive saliva-your body reacts to the foreign object. Drink water and it’ll pass.
- Tooth discomfort-pressure on front teeth is common. If it lasts beyond 4 weeks, your device needs adjustment.
Most dental sleep specialists recommend wearing the device for 1-2 hours during the day at first. This helps your jaw get used to the position. It’s not about snoring-it’s about training your muscles.
Don’t rush the titration. Most devices allow you to advance the jaw in 0.5mm increments. Go slow. Every 3-5 days, move it forward by one click. Stop when snoring drops significantly or when you feel discomfort. Pushing too hard too fast leads to failure.
Why Some People Fail-and How to Avoid It
Failure isn’t usually because the device doesn’t work. It’s because people don’t use it right-or they skip the follow-up.
Common mistakes:
- Buying an OTC device and expecting custom results
- Skipping the sleep study and assuming they have simple snoring
- Not adjusting the device after the first week
- Not cleaning it daily-bacteria build up fast
- Stopping use after a few nights because of discomfort
Success comes down to consistency. The 2021 Oral Sleep Appliance Network study found 76.4% of users were using their device nightly by day 30. Those who didn’t make it past week two rarely saw results.
And don’t underestimate the importance of fit. A 2022 study showed in-office digital scans produced a 23% better fit than at-home molds. That’s not a small difference-it’s the difference between relief and frustration.
The Future of Snoring Treatment
This field is evolving fast. In 2023, the FDA cleared the SomnoDent EVO 3, the first MAD with built-in sensors that track your snoring and jaw position in real time, sending data to your phone. By 2024, new devices will use AI to recommend personalized advancement settings based on your breathing patterns.
Harvard researchers are even studying genetic markers to predict who’ll respond best to MADs. The goal? No more trial and error. Just a scan, a test, and a device perfectly tuned to you.
For now, the best advice is simple: if you snore and want a non-invasive fix, talk to a dental sleep specialist. Don’t buy a cheap gadget off Amazon. Get evaluated. Get fitted. Give it time. It’s not magic-but for many, it’s the only thing that finally let them-and their partner-sleep through the night.
Are oral appliances better than CPAP for snoring?
CPAP stops snoring more effectively-85-95% of the time. But most people can’t stick with it. Oral appliances reduce snoring by 65-75% and have much higher long-term use rates (76% vs. 45%). If you can’t tolerate CPAP, MADs are the next best option.
Can I buy a mandibular advancement device online and skip the dentist?
You can, but you shouldn’t. Over-the-counter devices are less effective (48% reduction vs. 72% for custom), and they can damage your teeth or jaw if they don’t fit right. A dental sleep specialist ensures your device is safe, effective, and tailored to your anatomy.
How long does it take to see results with a MAD?
Most people notice less snoring within 1-2 weeks. But full adjustment takes 4-6 weeks, including gradual titration of the jaw position. Don’t expect overnight results. Patience and consistency matter more than speed.
Do oral appliances cause permanent dental damage?
About 25% of long-term users develop irreversible changes in their bite, such as tooth movement or jaw joint stress. That’s why regular dental check-ups every 6 months are essential. The risk is real-but manageable with proper monitoring.
Is oral appliance therapy covered by insurance?
Only about 38% of U.S. commercial insurance plans cover custom MADs. Medicare rarely does. You’ll likely pay out-of-pocket. Some providers offer payment plans. Always check with your insurer before starting treatment.
What happens if I stop using the device?
Snoring typically returns within 48 hours. MADs don’t cure the problem-they manage it. You need to use the device every night to keep your airway open. It’s not a one-time fix, but a long-term tool.


I tried one of those OTC gadgets after my wife threatened to sleep in the car 🤣 Honestly? It felt like chewing gum made of plastic bricks. But after 3 weeks of wearing it 1 hour a day first, it actually worked. No more pillow wars. Just me, my mouthguard, and sweet silence. 🌙💤
They’re hiding the real cost. Insurance won’t cover it because Big Dental and Big Sleep are in bed together. CPAP is a scam designed to keep you hooked. This jaw thing? It’s cheaper, quieter, and you don’t need a power outlet. Wake up.
There’s something deeply poetic about the idea that a tiny shift in your jaw-just 8 millimeters-can restore peace to a household. We spend so much money on pillows, sprays, and apps to fix sleep, but the real solution is anatomical. It’s not magic. It’s biology whispering back. And yet, we’re still surprised when it works. 🌿
In India, many still believe snoring is just ‘normal’-a sign of deep sleep. But I’ve seen friends with untreated sleep apnea develop hypertension, depression, even heart issues. This isn’t about comfort. It’s about survival. A custom MAD isn’t luxury-it’s preventive healthcare. If you can afford a smartphone, you can afford this. Your future self will thank you.
I got mine from a dentist who actually listens. Took 6 weeks. First week? Jaw felt like it was in a vise. Second week? I stopped noticing it. Now I forget I’m wearing it. The real win? My wife started sleeping through the night again. We’re both human now.
If you’re considering this, please don’t skip the sleep study. I did. Thought I just snored. Turns out I had 42 apneas an hour. MADs are great-but only if you know what you’re treating. Don’t guess. Get tested. You deserve to breathe.
OTC ones are a waste of money. I bought one off Amazon. It tasted like regret and plastic. My dentist laughed when I showed up with it. Said it looked like a child’s toy. Now I have a custom one. Worth every penny. And yes, my jaw hurts sometimes. But I’d rather have jaw pain than a wife who sleeps on the couch 😅
The biomechanical implications of mandibular advancement are non-trivial. The hyoid apparatus, genioglossus tone, and pharyngeal resistance dynamics are all modulated through anterior displacement. Long-term use induces neuroplastic adaptation in the motor cortex’s oromotor map. However, the 25% incidence of occlusal change suggests a potential maladaptive remodeling of the masticatory system. This necessitates longitudinal radiographic monitoring. The trade-off between symptomatic relief and structural alteration remains clinically ambiguous without individualized biomarker profiling.
I’ve been using mine for three years now. Honestly, I didn’t think I’d stick with it. But after the first month, I didn’t even notice it was there. The real surprise? I stopped waking up so tired. I used to need three coffees just to function. Now I’m up with the sun. My dentist says my teeth have shifted a bit-fair enough. But I’d rather have slightly crooked teeth than a partner who hates sleeping next to me. And yes, I clean it every night. No excuses. This thing saved my marriage more than any anniversary dinner ever could.