Penicillin Allergy Risk Checker
Check Your Reaction
This tool helps determine if your past penicillin reaction was likely a true allergy or just a side effect. Based on CDC guidelines and medical research, it assesses your risk level.
More than 10% of Americans say they’re allergic to penicillin. But here’s the truth: penicillin allergy is often misdiagnosed. Most people who think they’re allergic aren’t. They had a side effect - something uncomfortable, maybe scary - and labeled it an allergy. That mistake isn’t just inconvenient. It’s dangerous.
What’s the real difference between an allergy and a side effect?
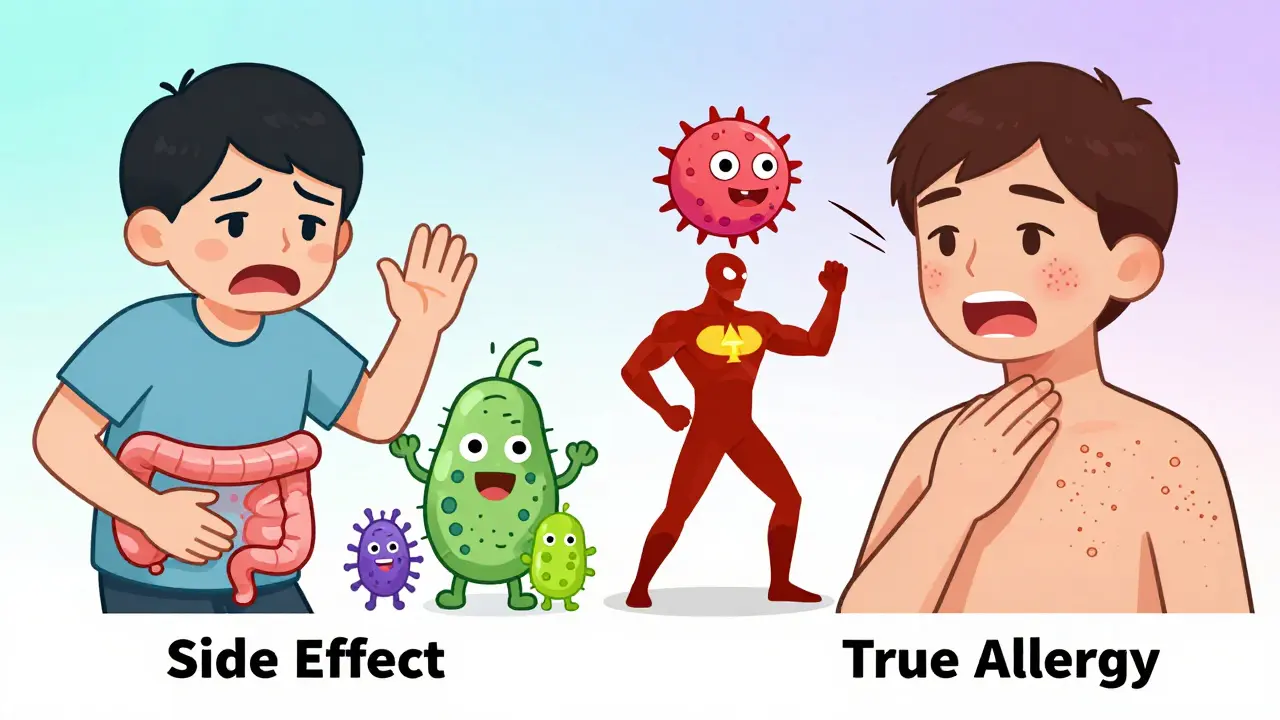
An allergy is your immune system overreacting. It sees penicillin as a threat and launches a full-scale response. That’s not just nausea or a rash - it’s your body attacking itself. A side effect? That’s your body simply reacting to the drug’s chemistry. No immune system involved. Just an unpleasant but harmless hiccup.
True penicillin allergies show up fast. Within minutes to an hour after taking the drug, you might break out in hives, your throat could swell, your blood pressure might drop, or you could start wheezing. These are signs of anaphylaxis - a life-threatening reaction. It’s rare, but it’s real. And if you’ve had one, you need to avoid penicillin forever.
But here’s where most people get it wrong. A rash that shows up three days after starting penicillin? That’s not an allergy. It’s a side effect. So is nausea, diarrhea, or a yeast infection. These happen because antibiotics disrupt your gut bacteria or irritate your stomach lining. They’re common - affecting up to 10% of people - but they’re not allergic reactions. And they don’t mean you can’t take penicillin again.
Why does this mistake matter so much?
If you’re labeled allergic to penicillin, doctors avoid it. They reach for something stronger - like vancomycin, clindamycin, or fluoroquinolones. These drugs are broader-spectrum. They kill more types of bacteria, but they also wreck your good bacteria. That’s why people with fake penicillin allergies are 45% more likely to get a C. diff infection - a nasty, sometimes deadly gut bug that thrives when antibiotics wipe out your natural defenses.
The cost isn’t just medical. A 2018 study in JAMA Internal Medicine found that patients with mislabeled penicillin allergies pay an extra $1,000 per hospital stay. They stay half a day longer on average. They’re more likely to get resistant infections like MRSA. And here’s the kicker: people with real penicillin allergies have a 6 in 1,000 higher chance of dying within a year of hospitalization than those who can safely use penicillin. Why? Because they’re stuck with weaker, riskier drugs.
Antibiotic resistance is growing. And this mislabeling is one of the biggest drivers. Every time we use a broad-spectrum antibiotic when we don’t need to, we help superbugs evolve. The CDC estimates this adds $20 billion to U.S. healthcare costs each year and creates 8 million extra hospital days.
Most people who think they’re allergic aren’t
Here’s the shocking part: less than 1% of people who say they’re allergic to penicillin actually are. That’s not a guess. That’s from clinical testing. The CDC says 33 million Americans claim a penicillin allergy. But only about 330,000 of them have a true IgE-mediated reaction.
Why the huge gap? Because most reactions were misinterpreted. A child gets a rash during a viral illness - maybe chickenpox or mono - and the doctor says, “Must be the penicillin.” Years later, that label sticks. Or someone had nausea once and never tried it again. Or a parent heard a story and assumed the worst.
And here’s something even more surprising: if you had a reaction more than 10 years ago, there’s an 80% chance you’re no longer allergic. Your immune system forgets. Penicillin-specific antibodies fade over time. That’s why so many people who get tested find out they’re fine.
How do you know if you’re really allergic?
Don’t rely on memory. Don’t trust a childhood note in your chart. Get tested.
The gold standard is a three-step process:
- History check - Your doctor asks detailed questions: When did the reaction happen? What did it look like? Did you need epinephrine? Was it within an hour? If it was a rash after three days, it’s likely not an allergy.
- Skin test - A tiny amount of penicillin is placed under your skin. If you’re allergic, you’ll get a red, itchy bump within 15 minutes. This test is over 95% accurate.
- Oral challenge - If the skin test is negative, you take a small dose of amoxicillin under observation. If you feel fine after an hour, you’re cleared.
These tests are safe. In a 2022 study at Mayo Clinic, over 52,000 patients went through this process. Not one had a serious reaction during the oral challenge. And 95% of those who were labeled allergic were cleared.
There’s even a tool called PEN-FAST that helps doctors decide if you’re low-risk. It asks five simple questions: Was the reaction fast? Did it involve breathing? Did you need treatment? Was it years ago? Did you have a rash? If your score is low, you’re a strong candidate for testing.
What’s stopping people from getting tested?
Mostly fear and access.
A 2021 survey found that 32% of people refused testing because they were scared of having a reaction. But the truth? The chance of a serious reaction during testing is less than 0.1%. You’re safer in a doctor’s office than you are taking a risky antibiotic at home.
Another big problem? Finding a provider who knows how to test. Many primary care doctors don’t offer skin tests. They don’t have the equipment. Or they don’t know the guidelines. One study found only 39% of primary care physicians knew that delayed rashes aren’t usually allergic.
Insurance can be a hurdle too. 45% of people who wanted testing couldn’t find an allergist covered by their plan. But things are changing. In 2023, Medicare raised reimbursement for penicillin skin testing by 37%. Hospitals are starting pharmacist-led programs. Kaiser Permanente now tests 15-20 patients a week with a 92% success rate.

What’s next? The future of penicillin allergy testing
Technology is helping. The CDC and University of Pennsylvania built a smartphone app called PAAT. You answer a few questions, and it tells you if you’re low-risk for testing. It’s 94% accurate. And as of 2024, Epic’s electronic health record system - used by 250 million Americans - now includes automatic alerts when a patient has a penicillin allergy label. It prompts doctors to consider testing.
By 2025, hospitals will be financially rewarded for reducing unnecessary antibiotic use. If you’re labeled allergic and you don’t get tested, your hospital could lose money. That’s a powerful incentive.
Experts predict that within five years, checking for penicillin allergy will be as routine as checking your blood pressure. If you’ve ever been told you’re allergic - even if it was decades ago - you should talk to your doctor about testing.
What to do if you think you’re allergic
If you’ve been told you’re allergic to penicillin, here’s your action plan:
- Look at your reaction. Was it a rash that showed up days later? Nausea? Diarrhea? That’s likely a side effect - not an allergy.
- Check when it happened. If it was more than 10 years ago, your chance of still being allergic is very low.
- Ask your doctor about penicillin skin testing. Don’t accept “just avoid it” as an answer.
- If your doctor doesn’t offer testing, ask for a referral to an allergist. It’s a simple, safe procedure.
- If you’re cleared, update your medical records. Tell every provider you see.
There’s no shame in being labeled allergic. But there’s huge value in being proven wrong. You might be able to take a safer, cheaper, more effective antibiotic. And you might just save your own life - or someone else’s - by helping slow the rise of superbugs.
Can you outgrow a penicillin allergy?
Yes. About 80% of people who had a true penicillin allergy as children or young adults lose their sensitivity after 10 years. The immune system stops producing the antibodies that cause the reaction. That’s why testing later in life is so important - you might be able to safely use penicillin again.
Is a rash always a sign of penicillin allergy?
No. A rash that appears days after starting penicillin is usually not an allergy. It’s often caused by a virus you already had, like Epstein-Barr or cytomegalovirus. Doctors used to blame the antibiotic, but now we know it’s usually unrelated. True allergic rashes show up fast - within minutes to an hour - and are often raised, itchy, and widespread.
What if I had anaphylaxis once? Can I ever take penicillin again?
If you had a true anaphylactic reaction - trouble breathing, swelling, drop in blood pressure - you should avoid penicillin for life. But even then, it’s worth confirming with testing. Some people who thought they had anaphylaxis actually had a severe side effect. Testing can rule out or confirm the diagnosis. Never assume - always get evaluated by an allergist.
Are there alternatives to penicillin if I’m truly allergic?
Yes. Cephalosporins (like cephalexin) are safe for most people with penicillin allergy - over 95% tolerate them without issue. Macrolides like azithromycin or tetracyclines like doxycycline are also good options. But the best alternative is penicillin itself - if you’re not truly allergic. Avoiding it unnecessarily leads to worse outcomes.
Can I get tested even if I’ve never had a reaction?
If you’ve never had a reaction but have a label in your chart from childhood, you can still be tested. Many people were labeled based on family history or a vague report. Testing can remove the label and open up better treatment options. You don’t need to have had a reaction to benefit from evaluation.


so like… i got a rash after amoxicillin when i was 7 and now im 32 and my doc just says ‘avoid penicillin’… but what if i’m not allergic anymore?? this article made me wanna cry… like, why did no one tell me i could get tested??
The misclassification of penicillin hypersensitivity as an IgE-mediated reaction is a pervasive diagnostic fallacy rooted in cognitive bias and inadequate clinical triage protocols. The majority of cutaneous eruptions occurring post-antibiotic administration are non-immunologic, often viral exanthems misattributed to pharmaceutical etiology. This epistemological error perpetuates suboptimal antimicrobial stewardship, increasing the incidence of C. difficile colonization and fostering multidrug-resistant organism selection pressure. Empirical avoidance of beta-lactams without confirmatory testing constitutes a form of therapeutic nihilism that directly compromises patient outcomes.
I love this so much. Seriously. I had a rash at 10, thought I was allergic, avoided penicillin for 20 years... then got tested last year and turned out I was fine. My doctor was shocked-I’d been labeled for life based on a childhood rash. Now I take amoxicillin for every sinus infection. It’s cheaper, better, and I don’t feel like I’m risking superbugs. Please, if you’ve been labeled, get tested. It’s not scary. It’s life-changing.
This is one of those quietly catastrophic public health issues that nobody talks about. The over-labeling of penicillin allergy isn't just a medical error-it's a systemic failure in communication, education, and follow-up care. And the consequences ripple outward: longer hospital stays, higher costs, increased resistance, and unnecessary suffering. The fact that 95% of those tested turn out not to be allergic speaks volumes. We need better protocols, better training, and better awareness-not just among patients, but among providers too.
My grandma was told she was allergic in the 50s. She never took penicillin again. Died of a bad infection in 2018 because they couldn’t use the best antibiotic. I cried reading this. If we’d known, we could’ve saved her. I’m getting tested next week.
STOP ACCEPTING LABELS WITHOUT QUESTION. If you’ve been told you’re allergic to penicillin, especially if it was decades ago or based on a rash that showed up days later-GET TESTED. It’s safe. It’s simple. It’s free or covered by insurance now. You’re not being dramatic. You’re being smart. And you might be saving your own life-or your kid’s life-down the line. Do it. Just do it.
The CDC’s assertion that less than one percent of self-reported penicillin allergies are true is statistically robust and corroborated by multiple peer-reviewed studies, including those published in JAMA Internal Medicine and The Lancet Infectious Diseases. The clinical utility of skin testing and oral challenge protocols exceeds 95% sensitivity and specificity. The persistence of this mislabeling phenomenon is therefore not attributable to diagnostic uncertainty, but rather to institutional inertia and inadequate physician education.
Wait-so if I had a rash after penicillin when I was 5, and I’m 40 now… I might be fine?? Like, I’ve been telling every doctor for 35 years, ‘I’m allergic!’… and I’ve been avoiding the best drug? That’s wild. I’m so mad I didn’t know this sooner. But also… kind of relieved? Like, my whole life I thought I was ‘that person’ who couldn’t take the easy fix. Turns out I just got bad info. Thanks for this.
Canada’s been doing this right for years. We have pharmacist-led allergy clinics in every major city. People get tested, get cleared, and their charts get updated automatically. Why is the U.S. still stuck in the 1980s? It’s not that hard. It’s not expensive. It’s just… laziness. We need policy change, not just education. Stop letting outdated labels kill people.
It’s fascinating how a single misdiagnosis, repeated across generations, becomes cultural dogma. We don’t question labels-we inherit them. Like religious beliefs passed down. And yet, the immune system isn’t static. It forgets. It adapts. It evolves. Maybe the real allergy here isn’t to penicillin-it’s to uncertainty. To not wanting to re-examine the stories we’ve been told. The science is clear. The question is: are we brave enough to unlearn?