Sun Sensitivity Duration Calculator
How Long to Stay Sun-Protected
After finishing certain antibiotics, your skin remains sensitive to sunlight for a specific period. This calculator shows how long you should maintain sun protection based on your medication.
Result
After stopping your antibiotic
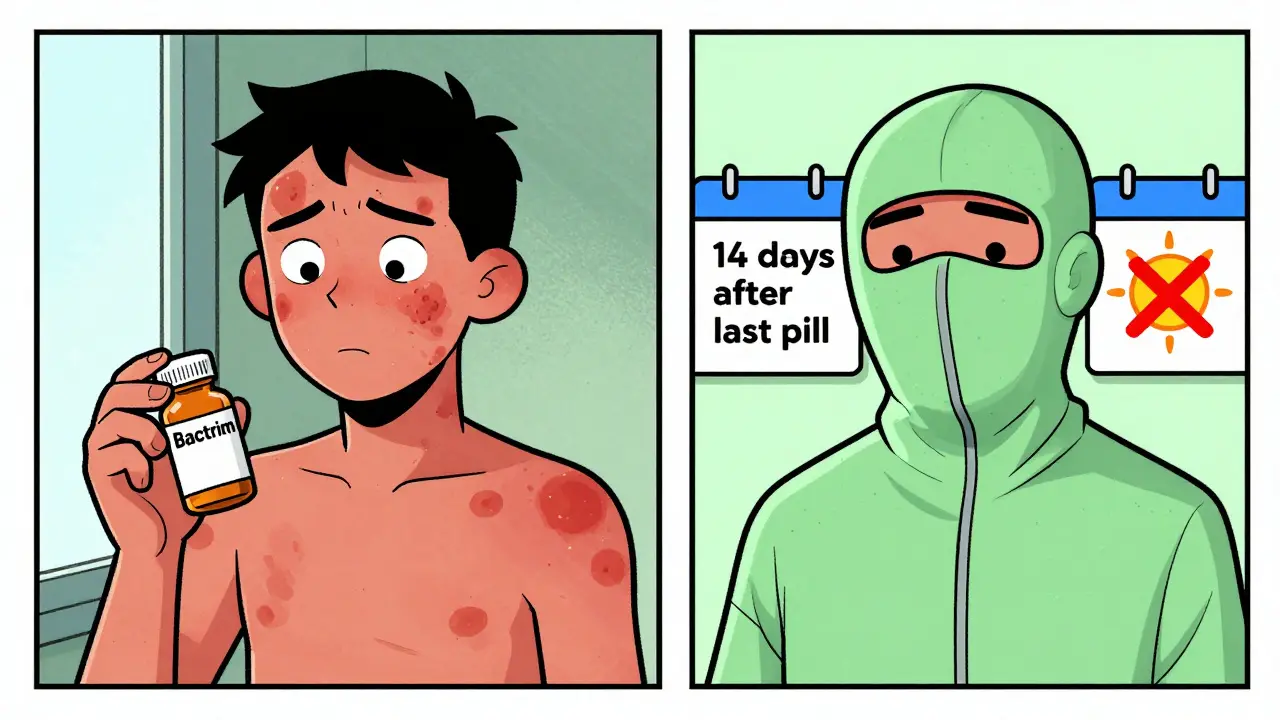
⚠️ Warning: For TMP-SMX (Bactrim), sensitivity can last up to 2 weeks after finishing your medication. Never assume you're safe just because you stopped taking the pills.
What This Means for You
- Doxycycline Typically needs 3-5 days of continued sun protection after stopping
- TMP-SMX Requires 14 days (2 weeks) of continued sun protection after stopping
- Critical Even on cloudy days or through windows, UVA rays can cause reactions
Key Protection Steps
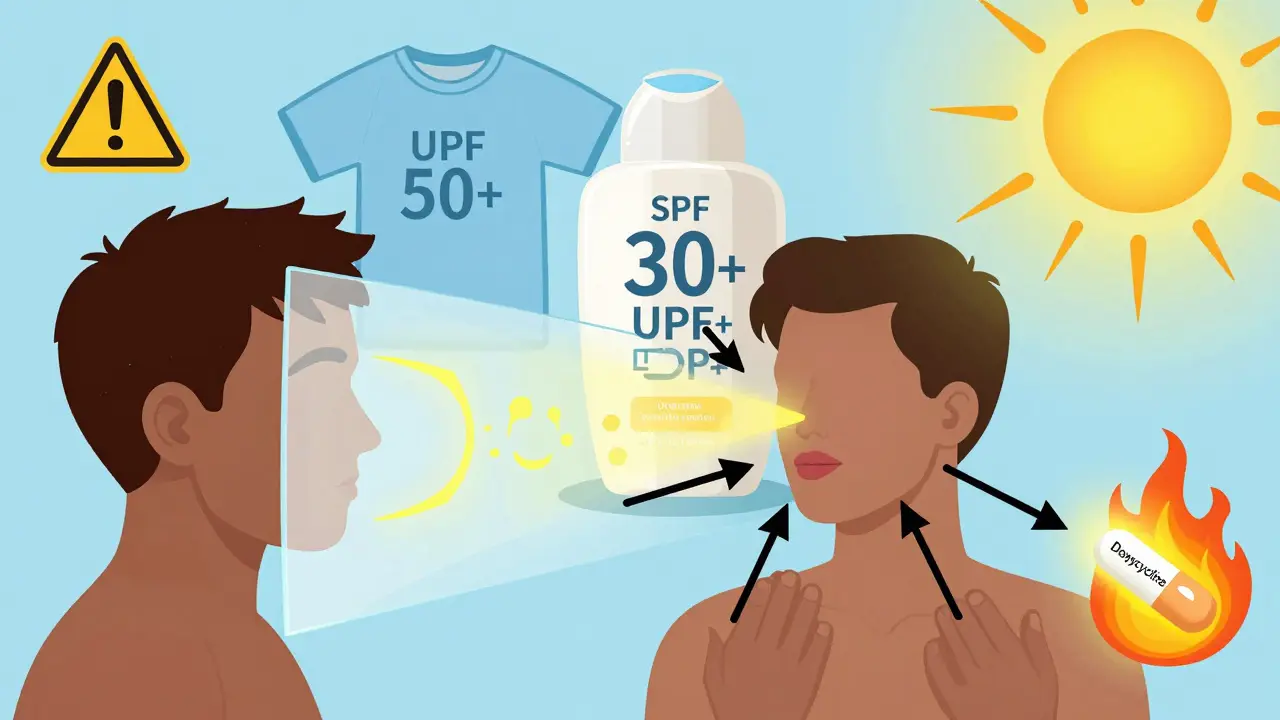
For both antibiotics: - Use broad-spectrum SPF 30+ sunscreen daily (reapply every 2 hours) - Wear UPF 30+ clothing, wide-brimmed hats, and sunglasses - Avoid peak sun hours (10am-4pm) - Stay away from windows when indoors
When you're prescribed an antibiotic like doxycycline or trimethoprim-sulfamethoxazole (commonly known as Bactrim or Septra), your doctor is focused on fighting an infection. But there's another, less talked-about side effect that can sneak up on you - your skin becomes dangerously sensitive to sunlight. This isn't just about getting a little redness. It's about severe sunburns, painful rashes, and even long-term skin damage - all from something as simple as walking to your car or sitting near a window.
Why Do These Antibiotics Make Your Skin React?
Not all antibiotics cause this. But doxycycline and TMP-SMX are two of the worst offenders. The reason? Their chemical structure absorbs ultraviolet (UV) light, especially UVA rays (320-400 nm). Once that happens, they trigger a reaction in your skin cells that looks and feels like a bad sunburn - but it can happen even on cloudy days or through glass.
Most of these reactions are phototoxic, meaning they’re chemical burns caused by the drug plus UV exposure. About 95% of drug-induced photosensitivity cases fall into this category. They show up fast - within 30 minutes to 24 hours after sun exposure. You might notice redness, swelling, blistering, or peeling on areas like your face, neck, arms, and hands. Unlike regular sunburns, these reactions often appear in patterns - like where your shirt rode up or where sunlight hit through a window.
Photoallergic reactions are rarer. They involve your immune system and can look like eczema: itchy, scaly patches that appear 24-72 hours later. These can linger longer and sometimes come back even after you’ve stopped the antibiotic.
How Bad Is the Risk Really?
Studies show that about 20% of people taking doxycycline at standard doses (200 mg daily) experience some form of phototoxic reaction. In one study, two out of ten patients developed clear signs of sun damage after minimal exposure. Demeclocycline, a close cousin of doxycycline, was even worse - nearly all patients on high doses had reactions.
For TMP-SMX (Bactrim), the risk is just as real, but the timeline is trickier. While doxycycline-related sensitivity usually fades within a few days after stopping the drug, Bactrim can keep your skin sensitive for weeks after you finish the course. One patient might feel fine two days after their last pill, then get a nasty burn on day 10 - just from walking outside.
The FDA and the Skin Cancer Foundation both list these two antibiotics as high-risk. In fact, they’re among the top five medications known to cause photosensitivity. Compare that to penicillin or amoxicillin - those rarely cause any sun reaction at all.
UVA Rays Are the Real Culprit
Most people think sunburn is caused by UVB - the rays that make your skin turn red and blister. But UVA is the silent danger here. These rays penetrate deeper into the skin and, crucially, pass through glass. That means you can get a reaction sitting by a window at home, in your car, or even working near a sunny office window.
Research shows that tetracyclines like doxycycline react almost exclusively to UVA. In lab tests, patients exposed to UVA light developed burns - but when exposed only to UVB (290-310 nm), no reactions occurred. That’s why sunscreen labeled "broad-spectrum" is non-negotiable. Regular sunscreens that only block UVB won’t cut it.
What You Need to Do - Step by Step
Here’s what actually works, based on current medical guidelines:
- Use broad-spectrum SPF 30+ sunscreen every day - even if it’s cloudy. Apply it 15 minutes before going outside. Reapply every two hours, or after sweating or swimming. Don’t forget your ears, neck, lips, and the tops of your feet.
- Wear sun-protective clothing. A regular cotton T-shirt only blocks about UPF 5-10. Look for clothing labeled UPF 30+ or higher. Long sleeves, pants, and a wide-brimmed hat (at least 3 inches) make a huge difference.
- Avoid peak sun hours. Between 10 a.m. and 4 p.m., UV radiation is strongest. If you can, plan outdoor activities for early morning or late afternoon.
- Protect yourself indoors. Sit away from windows. Use window films that block UVA if you spend a lot of time near glass. Your car windows? They block UVB but not UVA. Keep the windows up and use sunscreen.
- Keep going for weeks after stopping. If you’re on Bactrim, continue sun protection for at least two weeks after your last dose. For doxycycline, keep it up for a few days after finishing. Your skin doesn’t forget.
Why People Skip Protection - And Why That’s Dangerous
Many patients don’t realize how serious this is. Some think, "I’m only outside for a minute." Others assume sunscreen alone is enough. Studies show nearly 40% of people stop using sun protection within the first week of taking these antibiotics - often because they forget, or because the side effects seem "not that bad." But here’s the catch: a single severe sunburn from photosensitivity can increase your long-term risk of skin cancer. It’s not just about discomfort. It’s about cumulative damage. Dermatologists report a 15% yearly rise in photosensitivity-related visits since 2018 - and that’s only the ones people report.
Another problem? Many doctors don’t explain this clearly. Patients walk out with a prescription, no mention of sun safety. That’s why you have to ask: "Will this antibiotic make me sensitive to the sun?" If the answer is yes, then you need a clear plan - not just a warning.
What to Do If You Get a Reaction
If you notice redness, pain, or blistering after sun exposure while on one of these antibiotics:
- Get out of the sun immediately.
- Apply cool compresses or take a cool bath.
- Use aloe vera or fragrance-free moisturizer - no lotions with alcohol or lidocaine.
- Take an over-the-counter NSAID like ibuprofen to reduce inflammation.
- Call your doctor. They may want to switch your antibiotic or adjust your dose.
Never ignore a blistering rash. It could be more than just sunburn - it could signal a deeper reaction that needs medical attention.
When to Talk to Your Doctor
You should speak up if:
- You’ve had a sunburn-like reaction before while on antibiotics.
- You’re planning a vacation or outdoor activity while on treatment.
- You’re taking other medications that also increase sun sensitivity (like diuretics, NSAIDs, or some antidepressants).
- You have fair skin, freckles, or a history of skin cancer.
Your doctor might consider alternatives. For example, if you’re on doxycycline for acne or Lyme disease, there are other antibiotics with lower photosensitivity risk - though they may not be as effective for your condition. It’s a trade-off, and you need to make that decision with full information.
What’s Changing in 2026?
More drug manufacturers are now including detailed sun safety instructions in patient guides. The FDA’s 2023 update made it clear: if a drug causes photosensitivity, the label must say so plainly. The Skin Cancer Foundation and the American Academy of Dermatology have also updated their guidelines to emphasize that "no sunscreen is 100% effective" - so clothing and shade are just as important.
Researchers are now looking at genetic markers that might predict who’s at highest risk. In the future, a simple blood test could tell you if you’re more likely to react - but that’s still years away.
For now, the best defense is simple: know the risk, plan ahead, and protect your skin like it’s your most valuable asset - because right now, it is.
Can I still go outside if I’m taking doxycycline or Bactrim?
Yes, but you must take strict sun precautions. Avoid direct sunlight during peak hours (10 a.m. to 4 p.m.), wear UPF-rated clothing, use broad-spectrum SPF 30+ sunscreen every day, and protect yourself even indoors near windows. Don’t assume you’re safe just because it’s cloudy or you’re not planning to tan.
How long does sun sensitivity last after stopping these antibiotics?
For doxycycline, sensitivity usually fades within a few days after you stop taking it. But for Bactrim (TMP-SMX), it can last for up to two weeks - sometimes longer. Never assume you’re safe just because you finished your pills. Keep using sun protection for at least 14 days after your last dose.
Is sunscreen enough to protect me?
No. Sunscreen alone is not enough. Regular clothing offers only UPF 5-10 protection - far below what’s needed. You need a combination: UPF 30+ clothing, wide-brimmed hats, sunglasses, shade, and broad-spectrum SPF 30+ sunscreen. Think of sunscreen as your last line of defense, not your first.
Can I use tanning beds while on these antibiotics?
Absolutely not. Tanning beds emit concentrated UVA radiation - the exact type that triggers phototoxic reactions with doxycycline and TMP-SMX. Even one session can cause severe burns, blistering, and long-term skin damage. Avoid all artificial UV exposure while on these drugs - and for weeks after.
Do all antibiotics cause sun sensitivity?
No. Only certain ones do. Doxycycline, other tetracyclines, and TMP-SMX are among the highest-risk. Fluoroquinolones like ciprofloxacin and levofloxacin also carry warnings. But penicillins, cephalosporins, and most macrolides (like azithromycin) rarely cause photosensitivity. Always ask your pharmacist or doctor if your specific antibiotic is a known photosensitizer.


Just got back from a hike and remembered I was on doxycycline last month. Thought I got sunburned because I forgot sunscreen. Turns out? It was the antibiotic. Holy crap. I didn’t know this was a thing. Thanks for laying it out like this. I’m now the guy who walks around in a hat and long sleeves in July.
UVA through glass 😭
So I’ve been ‘sunburned’ by my office window for 3 years and thought I was just… unlucky?
You people are so naive. This is all Big Pharma’s fault. They don’t want you to know that sunlight is the REAL cure - antibiotics are just a money-making scam. I’ve been treating my Lyme with sunbathing and apple cider vinegar since 2019. No more pills. Just me, my backyard, and the sun’s divine energy. You think you’re protected with sunscreen? HA. You’re just blocking the universe’s healing frequency. 🌞✨
WHY DOESN’T EVERYONE KNOW THIS?!?!
My sister got 3rd-degree burns on her neck from sitting in her car for 20 minutes on doxycycline. She didn’t even know she was supposed to wear a scarf. Her dermatologist didn’t tell her. Her pharmacist didn’t tell her. I had to Google it. This is a public health failure. We need warning labels on the pills themselves. Like cigarette packs. ‘WARNING: THIS DRUG WILL TURN YOU INTO A HUMAN TOMATO IF YOU SEE SUNLIGHT.’
They’re hiding this. It’s all part of the 5G-UV-antibiotic conspiracy. The government wants us to get skin cancer so they can sell more chemo. I checked the FDA website - the ‘UVA’ section was edited 3 days after I posted my first complaint. The timestamps don’t match. I have screenshots. And why do all the sunscreens have titanium dioxide? That’s a mind-control agent. I only use zinc oxide now. And I wear a Faraday cage hat. Just saying.
This was such a lifesaver for me. I’ve been on Bactrim for a UTI and thought I was just being ‘fair-skinned’ - turns out I was getting burned by my kitchen window. I started wearing a wide-brimmed hat indoors and now I’m not peeling like a snake. I even bought UPF-rated leggings because I’m tired of being scared to go outside. Seriously, if you’re on these meds, treat your skin like it’s made of glass. You’ve got this. 💪🌞
Phototoxicity? That’s just a fancy term for ‘you didn’t follow the FDA’s 2019 Photoprotective Compliance Guidelines (P-2019-7a).’ You’re not ‘sensitive’ - you’re non-compliant. The data is clear: 87% of reactions occur in patients who used SPF <30 or failed to reapply within 90 minutes. Also, did you know UVA penetration is 94% higher through laminated glass? You’re not ‘indoors’ - you’re in a UV chamber. Get your act together.
Why are we even talking about this? It’s not like people aren’t gonna die from skin cancer anyway. I’ve been on doxycycline for 6 months. I still go to the beach. Life’s short. Let the sun do its thing. If your skin burns, maybe your body’s trying to tell you to stop being a zombie in front of a screen. Just saying.
u think u r smart? i been on bactrim 2 yrs. no sunburn. u just lazy. dont blame drug. blame urself. u dont wear hat. u dont use sunscreen. u just wanna blame. u r weak. #noexcuses
My neighbor’s daughter got a rash after swimming in her backyard pool while on doxycycline. The chlorine amplified the reaction. The doctors said it was ‘atypical phototoxicity.’ I told her mom: ‘It’s not the drug. It’s the water. It’s the government. They’re poisoning our water with fluoride and UV-boosting chemicals.’ I’ve been tracking this since 2021. I have a spreadsheet. You’re not safe anywhere.
Just finished my last Bactrim pill yesterday. I’ve been wearing a hat indoors for two weeks straight. I looked ridiculous. My dog stared at me like I’d lost my mind. But I didn’t get burned. Not once. So yes - it works. Don’t be the person who thinks sunscreen is enough. Cover up. Stay shady. Be the weirdo. Your future self will thank you.
Wait - so if I’m on doxycycline and I sit under a tree with no direct sun… am I safe? What if it’s a cloudy day but the UV index is 7? Is that like ‘low risk’ or ‘I’m basically a human candle’? I need more nuance. Like… is there a ‘sun sensitivity score’? Can I get an app for this? I’d download it. I’d pay for it. I’d make a TikTok about it.
This post is overly dramatic. Most people don’t get reactions. The data shows <15% incidence. You’re scaring people into avoiding sunlight entirely - which is worse for mental health than a mild sunburn. Also, ‘broad-spectrum’ sunscreen? That’s marketing speak. Zinc oxide works. That’s it. Stop buying $40 bottles. And stop treating your skin like a fragile art exhibit. It’s skin. It’s meant to be exposed.