When you’re pregnant, every pill, drop, or patch feels like a gamble. You take a pain reliever for a headache, maybe a cold medicine for a stuffy nose, or continue your antidepressant because stopping feels worse than risking the baby. But what if that medication could harm your unborn child? The truth isn’t black and white. Some drugs are known to cause serious birth defects. Others are safe-or at least safer than the illness they treat. And for many, we just don’t know for sure.
What Exactly Is a Teratogen?
A teratogen is any substance that can interfere with fetal development and lead to birth defects. It’s not just drugs-things like alcohol, tobacco, radiation, and certain infections can be teratogens too. But medications are one of the most common and controllable sources of risk. The term comes from the Greek word teras, meaning monster, and it’s not an exaggeration. In the late 1950s, the drug thalidomide, prescribed for morning sickness, caused over 10,000 babies worldwide to be born with missing or malformed limbs. That tragedy changed medicine forever. Today, we know that about 2-3% of all birth defects are linked to medications taken during pregnancy. That sounds low, but it’s not negligible. And the risk isn’t the same for every drug, or every stage of pregnancy. The most dangerous time is the first trimester-especially between weeks 3 and 8-when organs are forming. A medication that’s harmless in week 12 might be devastating in week 6.Medications with Proven Teratogenic Risks
Some drugs are so clearly dangerous that doctors avoid them entirely during pregnancy. Here are a few with strong evidence:- Warfarin (a blood thinner): Can cause fetal warfarin syndrome, which includes underdeveloped nasal bones, bone abnormalities, eye defects, and developmental delays. Risk is highest in the first trimester.
- Methotrexate (used for cancer and autoimmune diseases): A folate blocker that increases neural tube defect risk by 10-20%. Must be stopped at least 3 months before trying to conceive.
- Carbamazepine (for epilepsy): Carries a 1% risk of spina bifida and can cause vitamin K deficiency in newborns, leading to dangerous bleeding.
- Factor Xa inhibitors (rivaroxaban, apixaban, edoxaban): These newer blood thinners cross the placenta with no known antidote. No safe dose has been established.
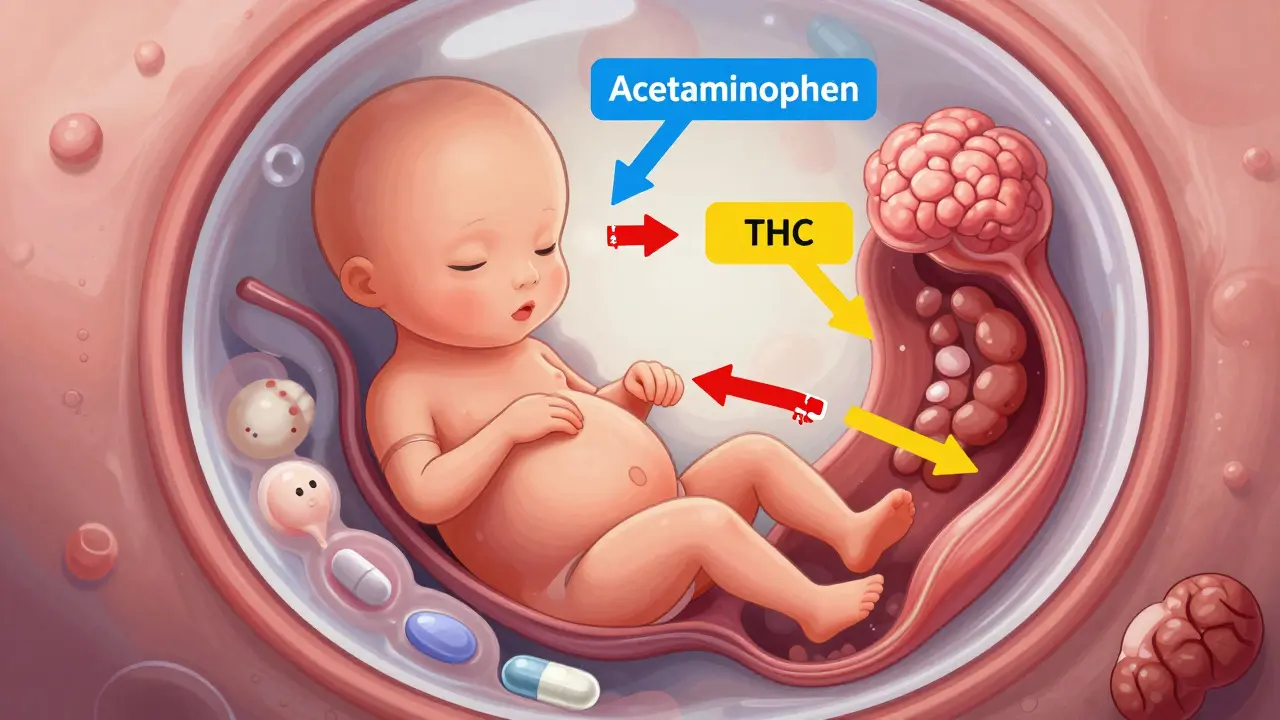
- Cannabis (THC): Linked to higher rates of low birth weight, preterm birth, and stillbirth. THC stays in breastmilk for days and may affect baby’s brain development.
The Acetaminophen Debate: Safe or Not?
No drug in pregnancy has sparked more confusion than acetaminophen (Tylenol). It’s the go-to for fever and pain. For decades, it was considered the safest option. But in recent years, studies have suggested a possible link to autism and ADHD when taken frequently during pregnancy. The CDC says some studies show an association. They don’t say it causes autism. They say there’s a signal worth watching. Meanwhile, the American College of Obstetricians and Gynecologists (ACOG) came out strongly in September 2025: “The conditions people use acetaminophen to treat during pregnancy are far more dangerous than any theoretical risks.” Untreated fever, for example, raises the risk of neural tube defects by 20-30%. Chronic pain can lead to depression, poor nutrition, and preterm labor. So who do you believe? The answer isn’t about picking a side. It’s about context. If you have a fever of 102°F, taking acetaminophen is likely protecting your baby. If you’re taking it daily for a chronic headache with no other treatment, that’s a different story. ACOG’s message is clear: don’t avoid acetaminophen out of fear. But don’t use it blindly either. Use the lowest dose for the shortest time needed.How Pregnancy Stages Change the Risk
It’s not just which drug you take-it’s when you take it.- Weeks 1-12 (First Trimester): This is the critical window for structural defects. The heart, brain, limbs, and organs are forming. A teratogen here can cause cleft palate, heart defects, or missing fingers.
- Weeks 13-26 (Second Trimester): Major organs are done forming, but the brain and genitals are still developing. Risk shifts toward functional problems-like hearing loss, learning delays, or genital abnormalities.
- Weeks 27-birth (Third Trimester): Structural defects are rare. But drugs can still cause problems: withdrawal in newborns (if mom used opioids), reduced fetal growth, or altered brain development. Some meds can trigger early labor.
How Medications Actually Harm the Fetus
Not all drugs work the same way. Here are the five main ways they can affect your baby:- No effect: About 60-70% of medications don’t cross the placenta or don’t harm fetal cells. Many antibiotics, antacids, and asthma meds fall here.
- Direct damage: The drug enters fetal cells and disrupts DNA or protein formation. Like methotrexate blocking folate needed for neural tube closure.
- Indirect harm: The drug lowers mom’s blood pressure so much that less oxygen reaches the placenta. This can stunt growth.
- Placental interference: Some drugs alter how the placenta works-reducing nutrient flow or increasing toxins.
- Uterine stimulation: Certain meds can trigger contractions, leading to preterm birth.
What You Should Do Before and During Pregnancy
You don’t have to guess. Here’s how to take control:- Review all meds before conception: Even over-the-counter pills, herbal supplements, and vitamins. Many women don’t realize that St. John’s Wort, high-dose vitamin A, or even some acne creams (like isotretinoin) are dangerous.
- Use reliable sources: Don’t trust Reddit threads or Google. Use MotherToBaby, the FDA’s Pregnancy and Lactation Labeling Rule (PLLR) on prescription labels, or LactMed (a free NIH database).
- Ask your pharmacist: Pharmacists are medication experts. They know which drugs cross the placenta, which have safer alternatives, and which are poorly studied.
- Don’t stop essential meds without help: If you have epilepsy, high blood pressure, or depression, stopping your meds can be more dangerous than keeping them. Seizures, strokes, or severe depression harm both you and your baby.
- Track your exposure: If you took a risky drug early on, write down the name, dose, and date. Share it with your OB. MotherToBaby handles over 10,000 calls a year from women just like you.
Why So Little Is Known
You might wonder: Why aren’t we sure about more drugs? The answer is simple: ethics. We can’t run clinical trials on pregnant women. We can’t randomly give some women a drug and others a placebo to see what happens. So almost all our data comes from:- Accidental exposures (women who didn’t know they were pregnant)
- Case reports (single stories of birth defects)
- Animal studies (which don’t always match human biology)
- Observational studies (tracking women who chose to take a drug)

The Future: Better Data, Better Choices
Change is coming. The FDA’s Sentinel Initiative is tracking 10 million electronic health records to find patterns in real time. By 2026, we’ll know faster if a new drug is risky. Researchers are also exploring pharmacogenomics-testing a woman’s genes to predict how she’ll metabolize a drug during pregnancy. One expert predicts this could improve personalized risk assessment by 30-40% in five years. But until then, the best tool you have is information-and a trusted medical team. Don’t suffer in silence. Don’t assume your OB knows every drug. Bring your pill bottles to appointments. Ask: “Is this safe? Is there a better option? What happens if I don’t take it?”Frequently Asked Questions
Can I take ibuprofen while pregnant?
Avoid ibuprofen after week 20. It can cause low amniotic fluid and kidney problems in the baby. Before week 20, occasional use is usually fine, but acetaminophen is still the preferred choice. Always check with your provider.
What if I took a risky medication before I knew I was pregnant?
Don’t panic. Most women who take a medication before realizing they’re pregnant go on to have healthy babies. The first 2-4 weeks after conception are a window where either the embryo survives unharmed, or it doesn’t. If your pregnancy continues past week 5, the risk of a major defect from that early exposure is very low. Talk to your doctor and get a detailed ultrasound at 18-22 weeks to check for structural issues.
Are antidepressants safe during pregnancy?
Some are, some aren’t. SSRIs like sertraline and citalopram are often considered the safest options for depression during pregnancy. Untreated depression raises the risk of preterm birth, low birth weight, and postpartum complications. Never stop antidepressants cold turkey-work with your psychiatrist and OB to find the lowest effective dose.
Is it safe to use nasal sprays or allergy meds?
Most saline sprays and antihistamines like loratadine (Claritin) and cetirizine (Zyrtec) are considered low risk. Avoid decongestants like pseudoephedrine in the first trimester-they can restrict blood flow to the placenta. Always check with your provider before using any nasal spray, even if it’s labeled "natural" or "herbal."
Why do different doctors give me different advice?
Because the science isn’t always clear. One doctor may rely on older studies showing a small risk. Another may follow ACOG’s 2025 guidance that prioritizes treating maternal illness. The key is to ask: “What’s the evidence behind your advice?” and “What happens if I don’t take this?” If you’re confused, ask for a pharmacist consult or call MotherToBaby for free, expert advice.


Stop panicking over every pill. If you’re taking meds for a real condition, stopping is way riskier than staying on them. Your kid’s not gonna turn into a monster because you took Tylenol once.
Dear friends, if you are pregnant and worried about medicine, talk to your doctor or pharmacist. Many medicines are safe. Even acetaminophen is okay if you use it only when needed. Don’t listen to scary stories online. Your health matters too.
The data on teratogenic risk remains fragmented due to systemic exclusion of pregnant populations from clinical trials. While anecdotal fear abounds, evidence-based guidance from ACOG and MotherToBaby should be prioritized over algorithmic sensationalism.
You got this. Every mom out there is scared, but you’re not alone. Talking to your doctor, reading real info, and taking one step at a time? That’s all it takes. You’re already doing better than most by even asking these questions.
The FDA and ACOG are complicit in a controlled narrative. Thalidomide was a cover-up. The real teratogens are pharmaceutical patents, not the drugs themselves. They suppress data on SSRIs and acetaminophen because profits outweigh fetal safety. Check the CDC’s hidden datasets - the correlation with autism is not "a signal," it’s a scream.
Listen - you’re not a bad mom for needing medicine. You’re a smart one for asking. I took Zyrtec, Tylenol, and sertraline through all three trimesters. My kid is 7 now, aced kindergarten, and still hugs me like I’m the best thing ever. You’re doing fine. Keep going.
How quaint. We’ve reduced the profound mystery of fetal development to a checklist of FDA-approved risk tiers. Meanwhile, the real tragedy isn’t the drugs - it’s that we’ve turned motherhood into a compliance test where your worth is measured by how well you follow the algorithm. Bravo, capitalism. Another baby, another data point.
It’s funny how we treat pregnancy like a chemical containment chamber - as if the body isn’t already a wild, messy, beautifully unstable ecosystem. We panic over acetaminophen like it’s poison, but ignore the real teratogen: chronic stress from being told you’re one wrong pill away from disaster. The real danger isn’t the medicine - it’s the guilt we’re fed like a daily supplement. You’re not a vessel. You’re a person. And your peace matters as much as your baby’s health.