When Your Skin and Joints Both Hurt
Imagine waking up with stiff fingers, swollen toes, and patches of scaly skin that burn or itch. You might think it’s just dry skin or a bad night’s sleep. But if you’ve had psoriasis for years, this could be something bigger: psoriatic arthritis. It’s not just a skin problem or a joint problem-it’s both. The same immune system glitch that causes red, flaky patches on your elbows or scalp is also attacking the lining of your joints. And if you ignore it, you could end up with permanent damage.
About 30% of people with psoriasis eventually develop psoriatic arthritis. That’s roughly 1 to 2 million Americans. For many, the skin comes first-those thick, silvery plaques on knees, scalp, or lower back. But in 15% of cases, the joints hurt before the skin shows any signs. That’s why doctors say: if you have psoriasis and your knuckles, knees, or heels start aching, don’t wait. Get checked.
How Psoriatic Arthritis Is Different
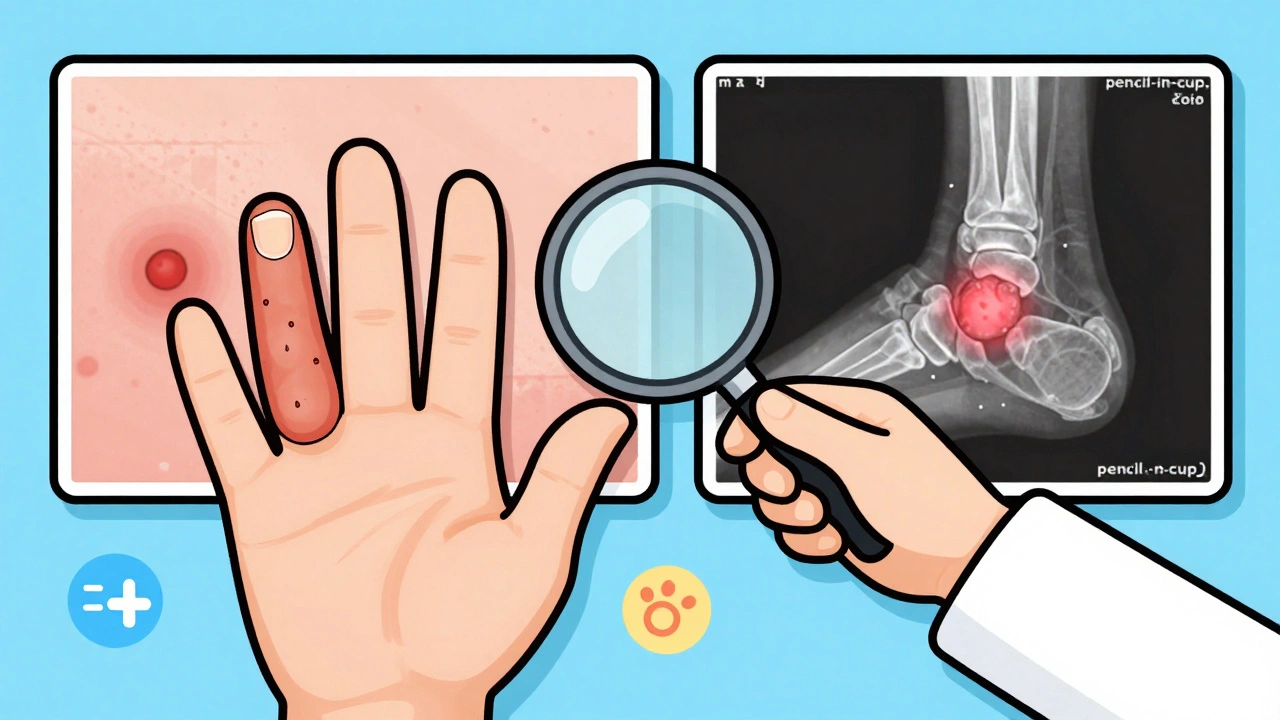
Not all arthritis is the same. Rheumatoid arthritis usually hits both sides of the body evenly-both wrists, both knees. Psoriatic arthritis? It’s messy. It might swell your right index finger and your left knee, but leave your left hand alone. This asymmetry is a red flag. So is dactylitis-when an entire finger or toe swells up like a sausage. That’s not just inflammation. That’s psoriatic arthritis showing its signature.
Another clue? Your nails. If you’ve noticed pits, ridges, or your nail pulling away from the bed, that’s not bad manicure habits. Eight out of ten people with psoriatic arthritis have these nail changes. In regular psoriasis alone, it’s only about half that rate. The immune system isn’t just hitting your skin-it’s hitting the nail matrix too.
And then there’s enthesitis. That’s when tendons or ligaments pull away from the bone. Think of it like fraying rope at the anchor point. It causes pain where your Achilles tendon meets your heel, or where your plantar fascia attaches to your foot. You might think it’s just plantar fasciitis. But if you also have psoriasis and joint pain, it’s probably psoriatic arthritis.
The Five Faces of Psoriatic Arthritis
This condition doesn’t show up the same way for everyone. There are five main patterns, and knowing which one you have helps guide treatment:
- Asymmetric oligoarthritis (70% of cases): Affects a few joints, not symmetrically. Often starts in fingers or toes.
- Symmetric polyarthritis (25%): Mimics rheumatoid arthritis-same joints on both sides. Harder to tell apart without blood tests.
- Distal interphalangeal predominant (5%): Hits the joints closest to the nails. Almost always comes with nail changes.
- Spondylitis (5-20%): Involves the spine. Can cause lower back stiffness, especially in the morning.
- Arthritis mutilans (less than 5%): The rarest and most destructive. Can cause bones to dissolve, leading to shortened fingers or toes.
Most people fall into the first two categories. But if your spine is stiff or your fingertips are crumbling, that changes the game. That’s why a rheumatologist needs to see your full picture-not just your joints, not just your skin, but both.
Why Diagnosis Takes So Long
On average, people wait over two years to get the right diagnosis. Why? Because there’s no single blood test for it. In rheumatoid arthritis, you can test for rheumatoid factor or anti-CCP antibodies. In psoriatic arthritis? Those markers are usually negative. Ninety percent of patients test negative. That means doctors can’t rely on labs alone.
Diagnosis comes from connecting dots: your skin history, joint pain pattern, nail changes, family history, and imaging. X-rays might show “pencil-in-cup” bone erosion in advanced cases. MRI or ultrasound can catch early inflammation in tendons and joints before it shows on X-rays. Many people are misdiagnosed with osteoarthritis or rheumatoid arthritis first. One Reddit user spent five years on the wrong meds before switching to ustekinumab and seeing 80% improvement.
And here’s the kicker: 45% of psoriatic arthritis cases are first spotted by dermatologists. If your skin doctor doesn’t ask about joint pain, you might slip through the cracks. That’s why it’s critical to tell your dermatologist if your joints ache-even if you think it’s “just aging.”
What Works: Treatments That Actually Help
Treatment has changed dramatically since the 2000s. Back then, doctors relied on methotrexate or sulfasalazine-drugs that helped some, but didn’t stop damage. Now, we have biologics and oral pills that target the exact parts of the immune system causing trouble.
Biologics are injectable or IV drugs that block specific inflammation signals. Examples:
- TNF inhibitors (adalimumab, etanercept, infliximab): First wave of biologics. Still widely used. Reduce joint swelling and skin plaques.
- IL-12/23 inhibitors (ustekinumab): Great for skin and joints. Helps with nail changes too.
- IL-17 inhibitors (secukinumab, ixekizumab): Fast-acting. Often clears skin in weeks.
- IL-23 inhibitors (guselkumab, risankizumab): Newer. Highly effective for both skin and joints. One patient reported morning stiffness dropped from two hours to 20 minutes in six weeks.
Oral options are growing:
- TYK2 inhibitors (deucravacitinib): First oral drug approved specifically for psoriatic arthritis in 2022. Works differently than older pills. No need for injections.
- JAK inhibitors (upadacitinib): Still in late-stage trials as of 2025. Could be a game-changer for those who hate needles.
Most patients need to try one or two drugs before finding what works. That’s normal. But don’t wait too long. Studies show if you start treatment within 12 weeks of symptoms, you can prevent irreversible joint damage in 75% of cases.
What You Can Do Every Day
Medications help-but they’re not the whole story. Lifestyle plays a huge role.
- Movement matters: Low-impact exercise like swimming, cycling, or yoga keeps joints flexible. Stiffness gets worse with inactivity.
- Weight control: Extra weight puts more stress on knees and feet. Losing even 10 pounds can reduce joint pain significantly.
- Quit smoking: Smoking makes inflammation worse and cuts the effectiveness of biologics.
- Watch your diet: No magic diet cures psoriatic arthritis, but reducing sugar, processed foods, and alcohol helps many patients feel better. Some report improvement with omega-3s and vitamin D.
- Track your triggers: Stress, infections, or even weather changes can spark flares. Keep a simple journal: what you ate, how you slept, how your joints felt.
Many patients say “brain fog” is one of the hardest parts. Even when joints feel better, mental fatigue lingers. That’s inflammation too-your brain is affected. Sleep hygiene, mindfulness, and talking to a therapist can help.

The Cost and the Challenge
Let’s be real: these drugs are expensive. Biologics can cost over $500 a month out of pocket-even with insurance. Many patients face 14-day delays getting approval from insurers. Some drop out of treatment because they can’t afford it.
But help exists. Patient assistance programs from drugmakers (like AbbVie, Janssen, and Pfizer) offer free or discounted meds to qualifying people. Nonprofits like the National Psoriasis Foundation can guide you through the process. Don’t give up because of cost. Ask your doctor. Ask your pharmacist. There’s almost always a path.
And yes, injections can be scary. Sixty-five percent of patients report injection site reactions-redness, itching, bruising. But most get used to it. Many clinics offer training sessions. You’ll learn how to do it yourself. It’s not as bad as you think.
What’s Next?
The future is looking brighter. AI tools can now predict who with psoriasis will develop arthritis-with 87% accuracy-using photos of nails and joint scans. That means we might be able to stop it before it starts.
By 2028, doctors may use genetic tests to match you with the best drug from day one. No more trial-and-error. No more two-year delays. Personalized medicine is coming.
And while there’s still no cure, the goal now isn’t just pain relief-it’s remission. Minimal disease activity. That means no swollen joints, no skin plaques, no fatigue. And with today’s treatments, 40-60% of patients reach that goal.
You’re not alone. Over a million Americans are managing this. You can too. The key is catching it early, staying on treatment, and speaking up when something’s wrong. Your skin and your joints are connected. So should be your care.
Can psoriatic arthritis develop without skin psoriasis?
Yes, in about 15% of cases, joint symptoms appear before any visible skin changes. This makes diagnosis harder, but if you have a family history of psoriasis or notice nail pitting, dactylitis, or enthesitis, it’s still likely psoriatic arthritis. A rheumatologist can confirm it with imaging and clinical signs.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. Rheumatoid arthritis usually affects joints symmetrically (both hands, both knees), and blood tests often show rheumatoid factor. Psoriatic arthritis is often asymmetric, involves entheses and nails, and typically has negative blood tests. Skin plaques and dactylitis are unique to psoriatic arthritis.
Do I need to see both a dermatologist and a rheumatologist?
Yes, ideally. Psoriatic arthritis affects both skin and joints, so care is best coordinated between a dermatologist (for skin and nails) and a rheumatologist (for joints and systemic inflammation). Studies show treatment plans involving both specialists are 85% more effective at controlling symptoms.
Can diet cure psoriatic arthritis?
No diet can cure it. But many patients report less inflammation and fewer flares when they reduce sugar, processed foods, alcohol, and saturated fats. Some benefit from omega-3 supplements or vitamin D. Diet supports treatment-it doesn’t replace it.
How soon should I start treatment after diagnosis?
Within 12 weeks. Research shows early treatment prevents irreversible joint damage in 75% of cases. Waiting increases the risk of permanent disability. Don’t delay-even if your symptoms feel mild.
Are biologics safe long-term?
Yes, for most people. Biologics are monitored closely for infections like tuberculosis or hepatitis before starting. Long-term data shows they’re generally safe and effective. The biggest risk is increased susceptibility to infections, which is manageable with screening and vigilance. The risk of not treating-joint destruction, disability-is far greater.
Will I need to take medication forever?
For most, yes. Psoriatic arthritis is a chronic condition. Some patients achieve deep remission and may reduce doses under doctor supervision, but stopping treatment usually leads to flare-ups. The goal is long-term control, not a cure. Think of it like high blood pressure-you manage it daily.
Next Steps
If you have psoriasis and joint pain:
- Write down your symptoms: Which joints hurt? When? How long does stiffness last?
- Check your nails: Are there pits, ridges, or separation from the bed?
- Ask your dermatologist: “Could this be psoriatic arthritis?”
- Request a referral to a rheumatologist. Don’t wait for your primary care doctor to bring it up.
- Bring your skin photos and joint pain log to your appointment.
If you’ve already been diagnosed:
- Track your flares. Note what triggers them-stress, sleep loss, illness.
- Ask about your treatment goal: Are you aiming for minimal disease activity?
- Find out if you qualify for patient assistance programs.
- Join a support group. You’re not alone.
The link between your skin and joints isn’t coincidence. It’s your immune system speaking. Listen. Act. Treat it early. Your future self will thank you.


This is just Big Pharma’s way of turning normal aging into a disease. I’ve had psoriasis for 20 years and my joints creak like an old floorboard-so what? They want you hooked on $10k/month injections so they can keep buying yachts.
Did you know the FDA approved biologics after being lobbied by shadowy biotech firms tied to the Illuminati? The nail pitting? That’s not inflammation-it’s a glyphosate signature. They’re hiding the truth because if you knew how much this was engineered, you’d never touch a drop of that ‘treatment’.
There’s something deeply human here-our bodies aren’t broken machines to be fixed with drugs, but systems trying to communicate. The skin and joints aren’t ‘linked’ by coincidence-they’re speaking the same language of stress, trauma, and systemic imbalance. Maybe we need to listen differently, not just inject more.
I had dactylitis for 18 months before anyone took me seriously. My doctor said it was ‘athlete’s foot with a bad attitude.’ I cried in the parking lot. Then I found a rheumatologist who actually looked at my nails. That was the day I stopped feeling like a hypochondriac and started feeling like a person. This post? It’s the reason I’m alive today.
OMG I JUST REALIZED MY NAILS ARE PITTIED 😭 I THOUGHT IT WAS BECAUSE I BIT THEM WHEN I WAS STRESSED BUT NOW I’M SCARED AND ALSO KINDA EXCITED BECAUSE I CAN FINALLY EXPLAIN WHY I’M ALWAYS TIRED 😭🙏 #PsAWarrior
If you have psoriasis and your knuckles hurt in the morning dont ignore it. I waited 3 years and now i have permanent damage in two fingers. The biologics worked but they dont reverse what was lost. Go see a rheum now. Your future self will beg you to have listened
I’m sorry, but this article is so overly optimistic. You mention ‘remission’ like it’s a given. But 60% of patients don’t reach it. And the cost? Most people can’t even afford the co-pay. You’re not helping-you’re gaslighting people into thinking it’s all fixable if they just ‘try harder.’
You wrote: 'The link between your skin and joints isn’t coincidence.' Correct. But you failed to cite the primary immunological pathways. The IL-23/Th17 axis is the mechanistic bridge-not a vague 'immune glitch.' Also, 'pencil-in-cup' is outdated terminology; it’s now 'marginal erosions with periosteal reaction.' Precision matters.
As a Nigerian-American woman who lived through both Western and traditional healing systems, I can tell you: this condition is not just medical-it’s cultural. In my community, we call it 'the body's cry.' We use turmeric, ginger, and prayer. But modern medicine saved my spine. Both worlds matter. Don’t dismiss one for the other.
I am from India and my father had this condition he never saw a doctor because he thought it was just dust allergy and joint pain from farming he died at 58 with fused spine and no diagnosis please dont make same mistake we need more awareness in developing countries
I’ve been on six different biologics. I cried the first time I got dressed without pain. Then I cried when my insurance denied the seventh. I’m tired. I’m not angry-I’m just… tired. This isn’t a battle. It’s a marathon with no finish line.
I’m a nurse who works with psoriatic arthritis patients. I’ve seen people go from wheelchairs to walking again. I’ve also seen people give up because they were told it’s 'just psoriasis.' This article is accurate, compassionate, and necessary. Thank you for writing it. If you’re reading this and hesitating-go. Now. Don’t wait.