People often assume that if something is natural, it’s safe. That’s one of the biggest mistakes you can make when it comes to your health. Whether you’re taking a prescription drug, an over-the-counter pill, or a daily herbal supplement, every substance you put into your body has the potential to cause harm. The truth is, medication and supplement risks aren’t just theoretical-they’re happening every day, in homes, hospitals, and emergency rooms across the country.
Supplements Aren’t Regulated Like Drugs
The U.S. Food and Drug Administration (FDA) treats dietary supplements like food, not medicine. That means companies don’t have to prove their products work before selling them. They also don’t have to prove they’re safe before putting them on shelves. All they need to do is report a problem after someone gets hurt. This system leaves a huge gap. In 2022 alone, the FDA received over 18,000 reports of adverse events linked to supplements. But experts say that’s likely just 1% of the real number-most people never report anything.
There are over 85,000 supplement products on the market today. You can buy them at the grocery store, the gym, or your favorite online retailer. But here’s the catch: many of these products contain ingredients that aren’t listed on the label. Some have hidden stimulants. Others have prescription drugs mixed in without your knowledge. In 2023, the FDA added 12 new high-risk ingredients to its advisory list, including bitter orange and yohimbe-both linked to heart attacks and strokes.
When Supplements and Medicines Collide
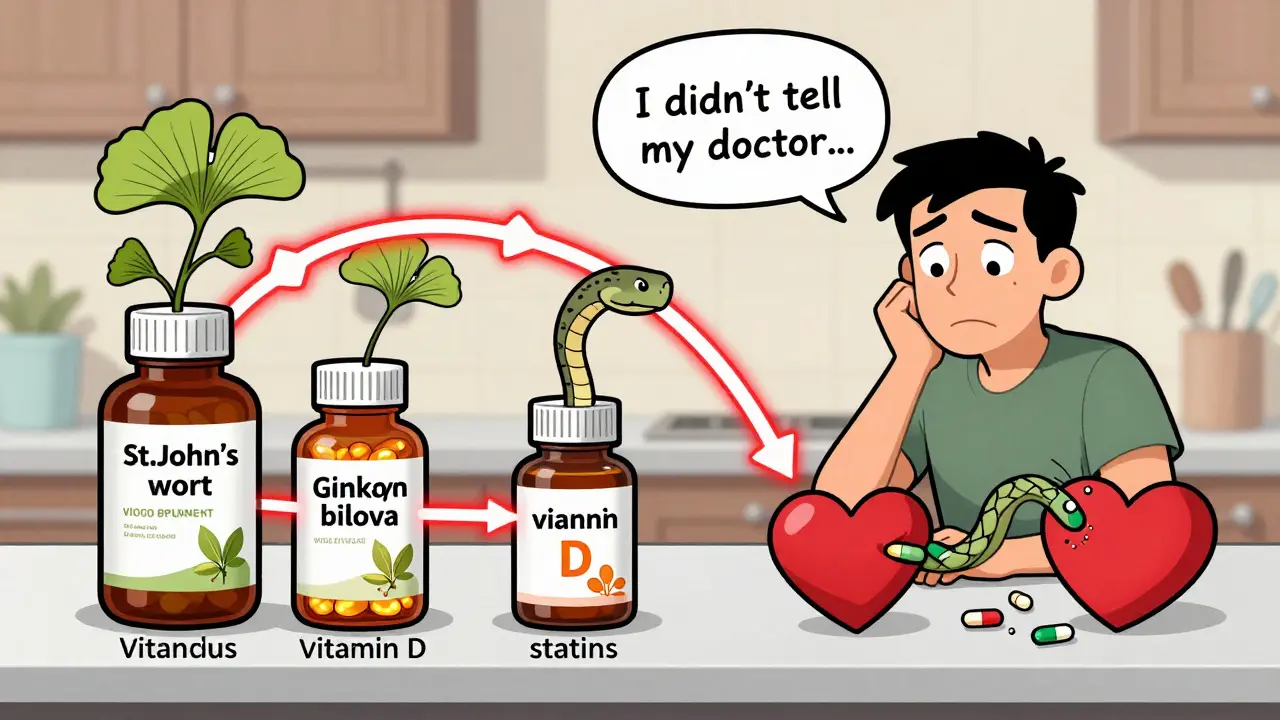
The real danger isn’t just what’s in the bottle-it’s what happens when supplements mix with your regular medications. These interactions can be silent, slow, and deadly.
Take St. John’s wort, a popular herb for mood support. It’s sold everywhere as a "natural antidepressant." But if you’re on birth control, it can cut the hormone levels in your body by 15%. That means you could get pregnant without realizing it. If you’re on chemotherapy, it can drop the drug’s effectiveness by up to 30%. If you’re taking cyclosporine after a transplant, it can slash your blood levels by 60%-and that can lead to organ rejection.
Goldenseal, another common supplement, interferes with how your liver breaks down drugs. It can make blood pressure pills, statins, and even HIV medications less effective. And ginkgo biloba? It’s marketed for memory, but it thins your blood. When taken with aspirin or warfarin, it can increase bleeding time by 20-30%. One 68-year-old woman ended up in the ER with internal bleeding after taking ginkgo with daily aspirin. She didn’t tell her doctor about the supplement. She didn’t know it was risky.
Even vitamins can be dangerous. Vitamin E at doses over 400 IU a day raises your risk of hemorrhagic stroke by 10%. Vitamin A, taken long-term at more than 10,000 IU daily, can damage your liver, blur your vision, and cause your skin to peel. Too much vitamin D? It can spike your calcium levels so high that you develop kidney stones, confusion, or even cardiac arrest.
High-Risk Groups and Hidden Dangers
Some people are at much higher risk. Older adults often take multiple medications and supplements at once. A 70-year-old man on blood thinners, a beta-blocker, and a statin might also be taking fish oil, garlic pills, and a multivitamin. That’s four different substances that can affect bleeding, heart rate, and liver function-all at once.
Cancer patients are another high-risk group. Antioxidants like vitamins C and E might sound like they help your body heal. But during chemotherapy or radiation, they can shield cancer cells from treatment. One radiation oncologist reported a patient had to pause treatment for three weeks because vitamin E caused severe skin burns during therapy. The American Cancer Society now advises cancer patients to avoid all supplements unless their oncologist specifically approves them.
And then there are the supplements you don’t even know you’re taking. Energy drinks? They often contain stimulants like caffeine and synephrine. Pre-workout powders? Some have hidden doses of DMAA, a banned substance linked to heart attacks. Even your "green tea extract" supplement could be damaging your liver. According to the Drug-Induced Liver Injury Network, green tea extract is responsible for 22% of supplement-related liver injuries.
What the Data Tells Us
The numbers don’t lie. In the U.S., dietary supplements cause about 23,000 emergency room visits every year. That’s more than all illegal drug overdoses combined. Herbal products-despite making up only 19% of supplement sales-account for 38% of adverse event reports. That’s because they’re complex. A single herb like ashwagandha can contain dozens of active compounds, each with its own effect on the body.
One Reddit user shared how taking 500mg of ashwagandha with their blood pressure medication led to severe insomnia and heart palpitations. Another reported that after taking a multivitamin with iron, they developed nausea, dizziness, and liver pain. These aren’t rare stories. They’re common.
The FDA’s own data shows that 45% of supplement-related problems come from products bought online. Why? Because online sellers aren’t required to test ingredients. There’s no guarantee what’s in the bottle. A 2022 study found that one in five supplements contained unlisted pharmaceuticals-like the same active ingredient found in Viagra or Adderall.

How to Protect Yourself
You don’t have to stop taking supplements to stay safe. But you do need to change how you think about them.
- Always tell your doctor about everything you take. That includes vitamins, herbs, protein powders, and even CBD oil. Studies show 67% of dangerous interactions happen because patients don’t disclose supplement use.
- Use a medication log. The NIH offers a free tool called "My Dietary Supplement and Medicine Record" that’s used by over 1,200 clinics. Write down every pill, capsule, and powder you take-and update it every time you see a provider.
- Be extra careful with high-risk combinations. Avoid St. John’s wort if you’re on antidepressants, birth control, or transplant meds. Don’t take vitamin K if you’re on warfarin. Stay away from ginkgo, garlic, or fish oil if you’re on blood thinners.
- Watch for red flags. If you start having unexplained rashes, heart palpitations, dizziness, or bleeding gums after starting a new supplement, stop it immediately and call your doctor.
- Report adverse events. If something goes wrong, file a report with the FDA through MedWatch Online. Your report could help prevent someone else’s tragedy.
The Bottom Line
There’s no such thing as a "harmless" supplement. Every pill you swallow has a biological effect. Some help. Some hurt. And some do both, depending on your health, your medications, and your dose. The idea that "natural" equals "safe" is a myth-and it’s costing people their health.
The safest approach isn’t to avoid supplements entirely. It’s to treat them like medicine. Ask questions. Check with your doctor. Track what you take. And never assume that because it’s sold on a shelf, it’s been tested for safety.
Are dietary supplements safer than prescription drugs?
No. Prescription drugs go through years of clinical testing before approval. Supplements don’t. Manufacturers aren’t required to prove safety or effectiveness. The FDA can only act after harm occurs, which often takes months or years. That delay means dangerous products stay on shelves while people get hurt.
Can I take supplements while on antibiotics?
Some can interfere. Probiotics are generally safe, but certain herbs like goldenseal and St. John’s wort can reduce antibiotic effectiveness. Others, like high-dose vitamin C or zinc, may alter gut bacteria in ways that affect how your body absorbs the drug. Always check with your pharmacist or doctor before combining supplements with antibiotics.
Why do supplements cause liver damage?
Many supplements contain plant extracts or concentrated compounds that the liver must process. Green tea extract, for example, can overload liver enzymes. Others contain heavy metals or contaminants from poor manufacturing. The NIH’s LiverTox database lists 45 supplement ingredients linked to liver injury. Green tea extract, weight-loss products, and bodybuilding supplements are the most common culprits.
Do multivitamins really help?
For most healthy people, no. Large studies have found no significant benefit in preventing heart disease, cancer, or cognitive decline. In fact, taking high doses of certain vitamins-like vitamin A, E, or beta-carotene-has been linked to higher mortality rates in some populations. If you’re not deficient, a multivitamin is unlikely to help and may even harm.
Can supplements interact with over-the-counter pain relievers?
Yes. Fish oil, garlic, and ginkgo biloba can increase bleeding risk when taken with aspirin or ibuprofen. Vitamin E at high doses can have the same effect. Even turmeric, often taken for inflammation, can increase the risk of stomach bleeding when combined with NSAIDs. If you’re taking pain relievers regularly, talk to your doctor before adding any supplement.
What should I do if I think a supplement made me sick?
Stop taking it immediately. Contact your healthcare provider. If you’re having serious symptoms like chest pain, difficulty breathing, or bleeding, go to the ER. Then, report the incident to the FDA through MedWatch Online. Your report helps the agency track dangerous products and protect others.


Been taking ashwagandha for months. Thought it was helping my anxiety. Then I started having heart palpitations at 3 a.m. Turns out it was messing with my beta-blocker. My doctor said I got lucky it wasn’t worse.
Now I log everything. Even the dumb stuff. No more guessing.
Supplements aren’t snacks. They’re chemicals. And your body doesn’t care if they’re ‘natural’ or not.
YESSSS this needs to be screamed from the rooftops 😭 I took a ‘natural energy booster’ last year and ended up in urgent care thinking I was having a heart attack. Turned out it had hidden caffeine and synephrine. My doctor looked at me like I’d just admitted to drinking gasoline.
STOP ASSUMING ‘NATURAL’ = SAFE. It’s not a yoga retreat. It’s pharmacology in disguise 🙃
As someone who works in integrative medicine, I see this daily. The biggest gap isn’t regulation-it’s patient communication. 70% of the folks I see don’t mention supplements because they think it’s ‘not medical.’
Here’s the reality: bioavailability, CYP450 interactions, hepatic metabolism-all these terms sound like jargon, but they’re why your statin stopped working or why your INR spiked. It’s not magic. It’s biochemistry.
Track. Disclose. Educate. Not because we’re scared of supplements-but because we’re scared of ignorance.
People who take supplements are just looking for shortcuts. You think you’re being smart by avoiding ‘pharmaceuticals’ but you’re just poisoning yourself with snake oil and wishful thinking. If you want to be healthy, eat real food, sleep, and move. Not pop pills labeled ‘ancient wisdom’ that have more chemicals than your phone charger.
Stop being gullible.
Oh, so now we’re blaming people for trusting the system that let them buy this stuff at Walmart next to the gummy vitamins? The FDA’s hands are tied. The industry’s a free-for-all. The real villain isn’t the consumer-it’s the $50 billion market that profits off ignorance.
And yes, I’m still mad they let ‘detox teas’ be sold as ‘weight loss aids’ while my actual prescriptions get scrutinized like contraband.
My PCP gave me a handout on supplement interactions last year. Honestly? It’s like a cheat sheet for avoiding ER visits.
St. John’s wort + birth control? Yeah, I didn’t know that. Ginkgo + aspirin? Nope, never connected the dots.
Now I show my doctor every bottle before I take it. Even the ‘harmless’ ones. Turns out, ‘harmless’ is just a marketing term.
Let’s clarify the liver damage point: green tea extract causes hepatotoxicity via catechin-induced mitochondrial dysfunction and oxidative stress in hepatocytes. The dose-response curve is non-linear-below 250mg EGCG, risk is negligible. Above 800mg daily, incidence spikes. Most commercial supplements contain 500–1000mg per serving.
Same with vitamin D: 2000 IU/day is safe. 10,000 IU/day? Hypercalcemia risk increases 8-fold. It’s not the supplement-it’s the dosing. And most people don’t know their own intake.
Knowledge > fear.
MY BEST FRIEND’S MOM DIED FROM A SUPPLEMENT INTERACTION. SHE TOOK GOLDENSEAL WITH HER BLOOD PRESSURE MEDS. NO ONE TOLD HER. NO ONE ASKED. SHE WAS 63. SHE WASN’T A FOOL. SHE WAS JUST TRUSTING THE SYSTEM.
THE FDA HASN’T SHUT DOWN A SINGLE SUPPLEMENT COMPANY SINCE 2019. NOT ONE. AND THEY STILL LET YOU BUY ‘TESTOSTERONE BOOSTERS’ THAT CONTAIN STEROIDS ON AMAZON.
THIS ISN’T A ‘RISK.’ IT’S A CRIME.
I used to think multivitamins were just ‘insurance.’ Now I know they’re just expensive urine.
My dad took one for 20 years. Got liver enzymes flagged last year. Turned out the iron and vitamin A were way over the RDA. He didn’t even know he wasn’t deficient.
Maybe the real takeaway is: if you don’t have a diagnosed deficiency, you probably don’t need it. Just… think before you swallow.