Serotonin Syndrome Risk Checker
This tool helps you understand the risk of serotonin syndrome when combining SSRIs and opioids. Select your current medications to get personalized safety information.
Every year, millions of people take SSRIs for depression or anxiety, and millions more get prescribed opioids for pain. It sounds simple enough - one pill for your mood, another for your back. But when these drugs meet in your body, something dangerous can happen: serotonin syndrome. It’s not rare. It’s not theoretical. It’s happening in hospitals, clinics, and homes right now - often missed, often misunderstood.
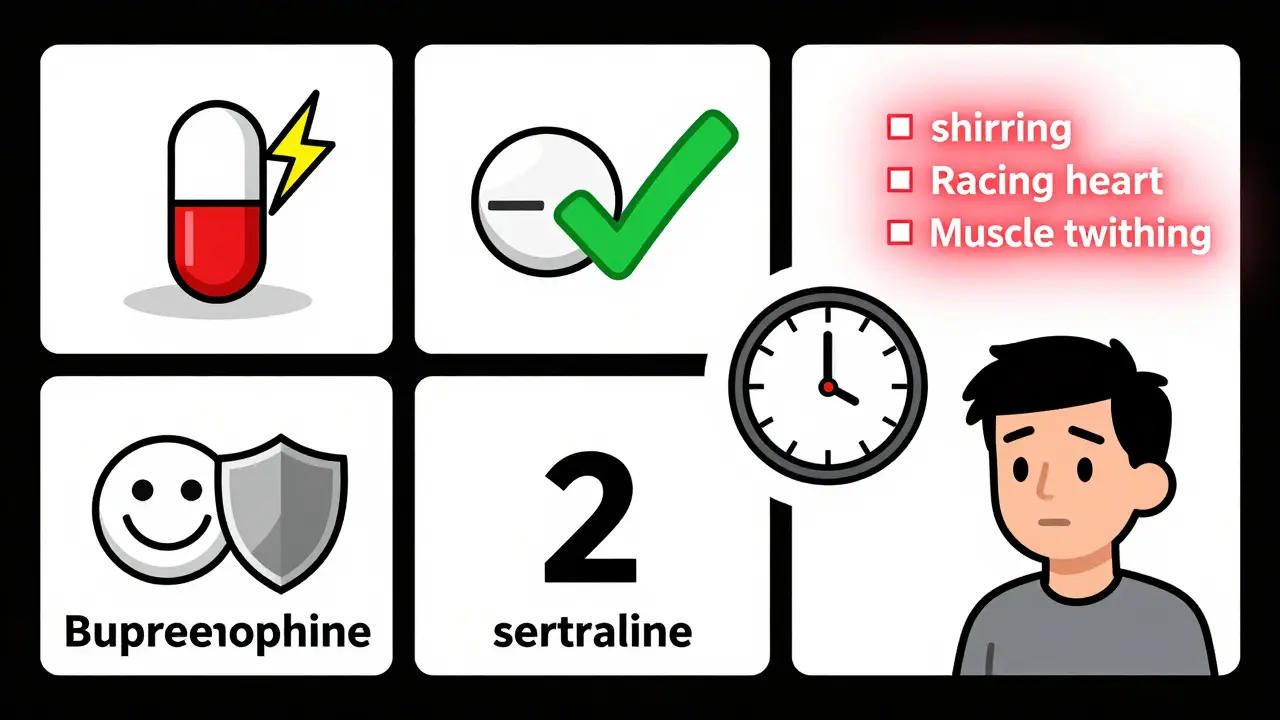
Imagine this: You’ve been on sertraline for six months. Your doctor adds tramadol after your knee surgery. Within 12 hours, you start shivering uncontrollably. Your heart races. Your muscles twitch. You feel like you’re burning up inside. You’re not having a panic attack. You’re not overdosing on painkillers. You’re experiencing serotonin syndrome - and it can kill you if no one recognizes it.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn’t an allergy. It’s not an overdose. It’s a biological cascade. Your brain and nervous system get flooded with too much serotonin - a chemical that helps regulate mood, sleep, and muscle control. When too much builds up, your body goes into overdrive. Think of it like a thermostat stuck on high. Your muscles spasm. Your heart pounds. Your temperature spikes. In severe cases, you can develop seizures, lose consciousness, or die.
The most reliable way to diagnose it? The Hunter Criteria. It’s not based on guesswork. It looks for specific signs: spontaneous muscle clonus (involuntary contractions), inducible clonus with agitation or sweating, or tremor with hyperreflexia. These aren’t vague symptoms. They’re measurable. And they show up fast - usually within hours of adding a new drug or changing a dose.
According to emergency department data, about 14-15% of people who overdose on serotonergic drugs develop serotonin syndrome. But here’s the scary part: most cases aren’t from overdoses. They’re from normal doses of two drugs that shouldn’t be taken together.
Which Opioids Are Dangerous With SSRIs?
Not all opioids are created equal when it comes to serotonin. Some are quiet. Others are loud.
High-risk opioids? Tramadol, methadone, and pethidine (meperidine). Why? They don’t just block pain. They also block the serotonin transporter - the system that normally clears serotonin from your synapses. Tramadol, for example, inhibits serotonin reuptake 30 times more strongly than morphine. That’s not a small effect. It’s enough to push someone over the edge, especially if they’re already on an SSRI like fluoxetine or sertraline.
Studies show tramadol combined with SSRIs carries a 4.4 times higher risk of serotonin syndrome than morphine with SSRIs. The FDA recorded 848 cases of serotonin syndrome involving opioid-SSRI combinations between 2018 and 2022. Tramadol was involved in 37.2% of them.
On the other hand, morphine, oxycodone, buprenorphine, and hydromorphone? They barely touch serotonin. They’re much safer choices if you need an opioid while on an SSRI. You don’t need to avoid opioids entirely - just avoid the ones that play with your serotonin system.
Which SSRIs Are the Worst Offenders?
Not all SSRIs are equally risky. Fluoxetine is the troublemaker. Why? Because it sticks around. Its half-life is 2-4 days. Its active metabolite, norfluoxetine, lasts 4-16 days. That means if you stop fluoxetine, your body is still flooded with serotonin for weeks. If you start an opioid during that time - even a week later - you’re still at risk.
Sertraline? Half-life is about 26 hours. Much safer to switch. Citalopram and escitalopram? Moderate risk. Paroxetine? It’s a strong inhibitor of liver enzymes, which can slow down how fast other drugs are broken down. That adds another layer of risk.
And don’t forget SNRIs. Venlafaxine and duloxetine are even riskier than most SSRIs because they affect both serotonin and norepinephrine. If you’re on one of those and an opioid like tramadol? You’re in the danger zone.

Real Cases. Real Consequences.
A 68-year-old woman in Boston was on sertraline for depression. After her hip replacement, her surgeon prescribed tramadol for pain. Twelve hours later, she was in the ER with a temperature of 40.2°C (104.4°F), a blood pressure of 180/100, and spontaneous clonus. She survived - but barely. Her kidneys were strained. Her muscles were damaged. She spent five days in the ICU.
Another case? A 52-year-old man on paroxetine started taking codeine for a dental procedure. Doctors thought codeine was safe. It’s not. A 2018 case report in the Canadian Pharmacists Journal showed codeine triggered serotonin syndrome in someone already on an SSRI. That case shattered old assumptions.
Hospital pharmacists in major U.S. cities report seeing 2-3 cases per month. Most are in post-op patients. Most involve tramadol. And most are misdiagnosed - confused for neuroleptic malignant syndrome, sepsis, or even a panic attack. Delayed treatment means worse outcomes.
How to Prevent It
Prevention isn’t about fear. It’s about smart choices.
- Avoid high-risk combinations entirely. If you’re on an SSRI or SNRI, don’t take tramadol, methadone, or pethidine. Period. There are safer painkillers.
- Choose safer opioids. Morphine, oxycodone, hydromorphone, and buprenorphine have minimal serotonin activity. Ask your doctor if one of these can work instead.
- Wait before switching. If you’re stopping fluoxetine, wait at least 5 weeks before starting an opioid. For other SSRIs, wait 2 weeks. Don’t guess - check with your pharmacist.
- Use electronic alerts. Hospitals like Kaiser Permanente cut inappropriate tramadol-SSRI prescriptions by 87% after adding hard stops in their EHR systems. Ask your provider if their system has these safeguards.
- Know the warning signs. Shivering you can’t stop. Muscle twitching. Rapid heartbeat. Sweating. Agitation. Confusion. High fever. If you feel any of these after starting a new pain med, stop the opioid and get help immediately.
Patients should be given a simple checklist: “If you feel like you’re burning up inside, your muscles are jumping, or your heart won’t slow down - call your doctor or go to the ER. Don’t wait.”
What If It Happens?
If serotonin syndrome is suspected, stop all serotonergic drugs immediately. No exceptions. No “wait and see.”
For mild cases: supportive care. Cool the body. Give fluids. Use benzodiazepines to calm muscle spasms and agitation. Most people recover in 24-72 hours.
For severe cases: cyproheptadine. It’s an antihistamine that blocks serotonin receptors. The standard dose? 12 mg orally, then 2 mg every 2 hours until symptoms improve. In critical cases, ICU care, intubation, and cooling blankets are needed. Mortality in untreated severe cases? Up to 10%.
There’s no antidote. No magic pill. Just early recognition and fast action.
Why This Is Getting Worse
Between 2017 and 2022, serotonin syndrome cases increased by 34.7%. Why? Because more people are on antidepressants. More people are on opioids. And more doctors are prescribing them together without realizing the risk.
One in five opioid prescriptions in 2022 went to someone already taking an antidepressant. That’s 15 million people in the U.S. alone. And the aging population? They take 31.4% more medications than younger adults. More drugs. More interactions. More risk.
Regulators are catching up. The FDA updated opioid medication guides in 2022 to include serotonin syndrome warnings. The European Medicines Agency now requires stronger labels on tramadol. But guidelines aren’t enough. We need systems that stop these combinations before they happen.
Next year, Epic Systems - the biggest EHR platform in the U.S. - will roll out tools that check for 17 genetic and drug interactions linked to serotonin metabolism. That’s progress. But until then, the burden is on you and your doctor to know the risks.
Final Thoughts
You don’t need to avoid pain relief. You don’t need to stop your antidepressant. But you do need to know which drugs are safe together - and which are a ticking time bomb.
Tramadol isn’t evil. SSRIs aren’t dangerous. But together? They can be deadly. The science is clear. The cases are documented. The prevention strategies work.
If you’re on an SSRI and need pain relief, ask: “Is there a safer opioid?” If your doctor says tramadol is fine - get a second opinion. If you’re feeling strange after starting a new pain med - don’t brush it off. Call your pharmacist. Go to urgent care. It’s better to be safe than sorry.
Serotonin syndrome isn’t a myth. It’s a preventable emergency. And knowing the difference could save your life - or someone else’s.

