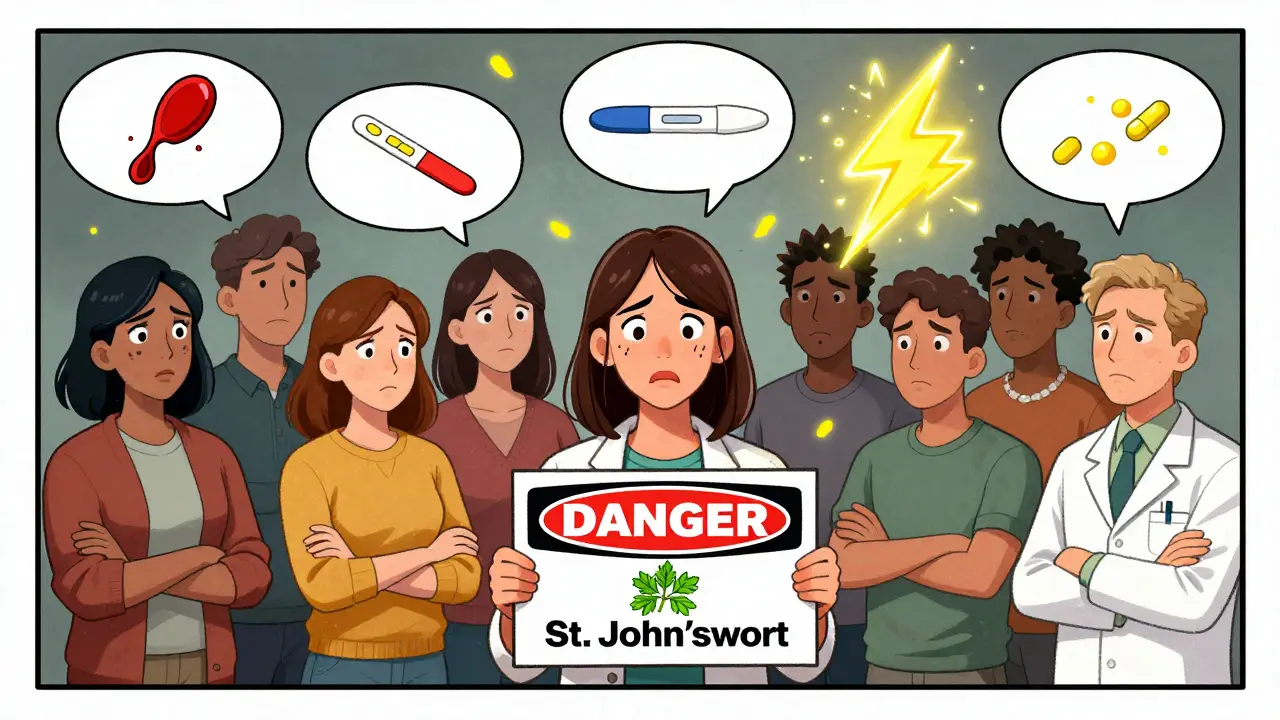
St. John’s Wort might seem harmless-a natural remedy for low mood, sold next to vitamins in grocery stores and online. But here’s the truth: it’s not just another supplement. It’s a powerful biological actor that can turn life-saving medications into useless ones. If you’re taking warfarin, birth control, an HIV drug, or even an antidepressant, St. John’s Wort could be quietly sabotaging your treatment-and you might not even know it.
How St. John’s Wort Changes Your Body’s Chemistry
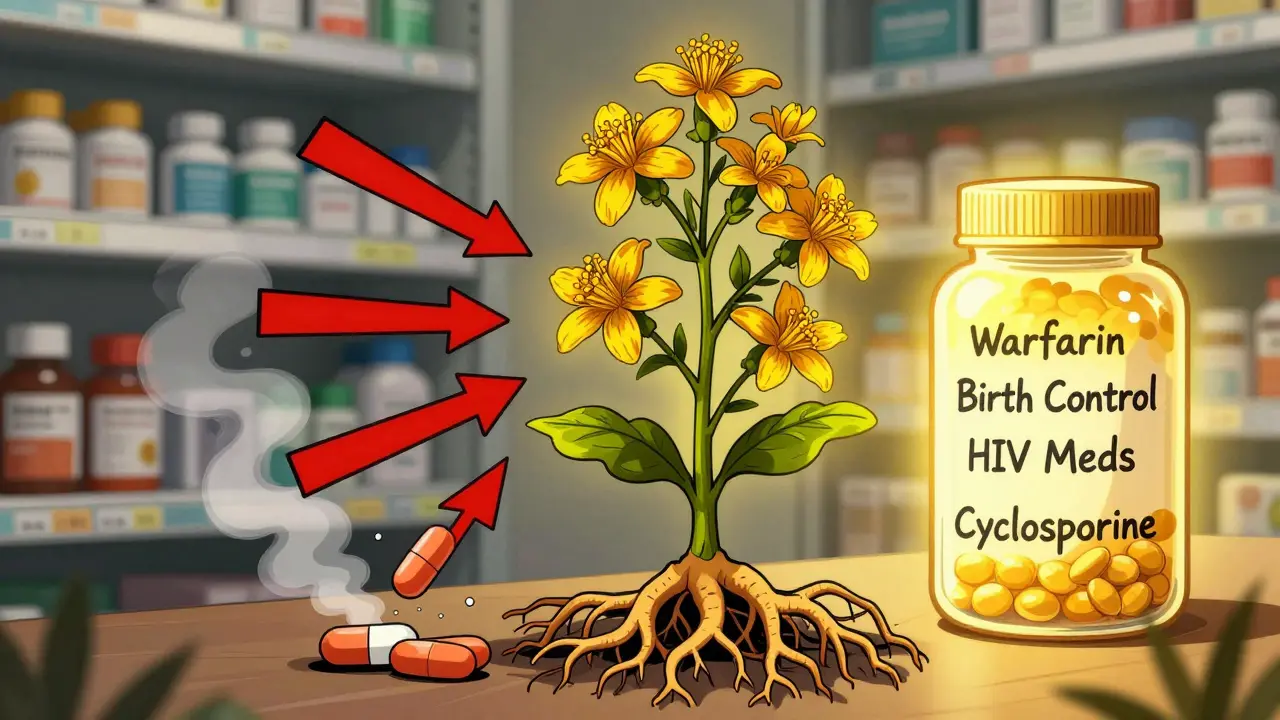
St. John’s Wort doesn’t just sit there. It actively rewires how your body processes drugs. The key player is a compound called hyperforin, found in the plant’s flowers and leaves. Hyperforin turns on a switch in your liver called the pregnane-X-receptor (PXR). Once flipped, this switch tells your body to make more of two powerful enzyme systems: CYP3A4 and P-glycoprotein. These systems are like the body’s trash disposals for drugs. When they’re turned up, they break down and flush out medications faster than normal. That means less of the drug stays in your bloodstream. For some medicines, even a small drop can be dangerous. A 2006 study showed that standard St. John’s Wort extracts-those with 3-5% hyperforin-can boost CYP3A4 activity by 2 to 3 times within just two weeks. That’s not a minor change. It’s the same level of enzyme induction as strong prescription drugs like rifampin. And here’s the kicker: the effect doesn’t disappear the day you stop taking it. It lingers for up to two weeks. That means if you quit St. John’s Wort and then start a new medication, your body might still be processing it too fast.Warfarin and Blood Thinners: A Silent Risk
If you’re on warfarin (Coumadin) or phenprocoumon (Marcoumar), St. John’s Wort can be deadly. These drugs keep your blood from clotting too easily. But St. John’s Wort speeds up their breakdown. Your INR-a measure of how long it takes your blood to clot-plummets. That means clots can form without warning. Between 1998 and 2000, European health agencies recorded 22 cases where people on warfarin started taking St. John’s Wort and suddenly developed dangerous clots. One case involved a 62-year-old man whose INR dropped from 2.8 to 1.4 in just seven days. That’s not a glitch. That’s a medical emergency. His risk of stroke or pulmonary embolism skyrocketed. Phenprocoumon isn’t safe either. One study found that patients taking 900 mg of St. John’s Wort daily saw their phenprocoumon levels drop by 37%. No warning. No symptoms. Just a blood test that shows your medicine isn’t working anymore.Organ Transplants at Risk
For people who’ve had kidney, liver, or heart transplants, St. John’s Wort is a dealbreaker. Immunosuppressants like cyclosporine and tacrolimus are the lifeline that keeps the body from rejecting the new organ. But St. John’s Wort slashes their levels. A 2004 study tracked 10 kidney transplant patients who added St. John’s Wort to their regimen. Cyclosporine levels dropped by 54%. Two of them had acute transplant rejection-meaning their bodies attacked the new organ. One patient lost the transplant. The European Medicines Agency reviewed 17 similar cases and issued a formal warning. Tacrolimus isn’t any safer. Levels can fall by up to 60%. There’s no safe dose. No monitoring trick. If you’ve had a transplant, don’t touch St. John’s Wort. Period.HIV Medications: A Recipe for Resistance
St. John’s Wort doesn’t just reduce HIV drug levels-it can make them useless. Protease inhibitors like indinavir are especially vulnerable. A 2004 clinical study found that St. John’s Wort cut indinavir’s concentration in the blood by an average of 57%. In some people, it dropped by nearly 99%. That’s not just a drop in effectiveness. That’s a direct path to drug-resistant HIV. When the drug level falls below the threshold needed to suppress the virus, the virus mutates. Those mutations stick. They spread. And suddenly, your entire treatment plan collapses. A UK case report documented a patient whose HIV viral load spiked after starting St. John’s Wort. He had been undetectable for years. Within months, his virus was replicating again. The U.S. Department of Health and Human Services explicitly says: Do not use St. John’s Wort with any HIV medication.
Birth Control Failure: Real Pregnancies, Not Just Theories
Many women assume herbal supplements are safe during hormonal birth control. They’re wrong. St. John’s Wort reduces the levels of ethinyl estradiol and levonorgestrel-the two hormones in most pills-by 15% and 26%, respectively. That’s not theoretical. Between 2000 and 2003, Sweden’s medical agency recorded 47 cases of contraceptive failure linked to St. John’s Wort. Twelve of those were confirmed pregnancies. GoodRx’s 2022 analysis of FDA reports found 217 cases of possible birth control failure tied to this herb. You might not know you’re at risk. You might think, “I’ve been taking this for years.” But St. John’s Wort doesn’t care about your history. It only cares about the enzymes it turns on. Even if you’ve taken it before without issue, the next time could be the one that changes your life.Antidepressants and Serotonin Syndrome
If you’re on an SSRI like fluoxetine (Prozac) or sertraline (Zoloft), or an SNRI like venlafaxine (Effexor), mixing it with St. John’s Wort is like pouring gasoline on a fire. Both raise serotonin levels. Together, they can cause serotonin syndrome-a rare but life-threatening condition. Symptoms show up fast: sweating, rapid heartbeat, muscle spasms, confusion, high blood pressure. In one 2021 case, an 18-year-old man developed paranoid delusions, a heart rate of 128 bpm, and blood pressure of 162/98 after combining St. John’s Wort with 5-HTP, melatonin, and Adderall. He ended up in the ER, needing IV fluids and benzodiazepines to calm his nervous system. The American Psychiatric Association says if you’re switching from an antidepressant to St. John’s Wort, wait at least 14 days. That’s not a suggestion. That’s a safety rule. Go sooner, and you risk poisoning your own brain chemistry.Other Dangerous Interactions
St. John’s Wort doesn’t stop there. - Benzodiazepines like alprazolam (Xanax): Levels drop by 40%. Anxiety returns, harder than before. - Digoxin (Lanoxin): Used for heart failure. Levels fall by 25%. Heart rhythm gets unstable. - Phenytoin (Dilantin): An antiseizure drug. Levels drop 19-46%. Seizures return. The FDA logged 12 such cases between 2000 and 2005. These aren’t rare. They’re predictable. Every time someone takes St. John’s Wort with one of these drugs, the outcome follows the same pattern: the medication stops working, and the patient suffers.