Why Rifampin Is Both a Lifesaver and a Hidden Risk in TB Treatment
When you hear about tuberculosis treatment, you might think of a simple six-month course of pills. But behind that routine is a powerful drug with a dangerous secret: rifampin doesn’t just kill TB bacteria-it rewires your body’s ability to process almost every other medication you take. This isn’t a minor caution. It’s a full-system override that can turn a safe drug into a life-threatening one.
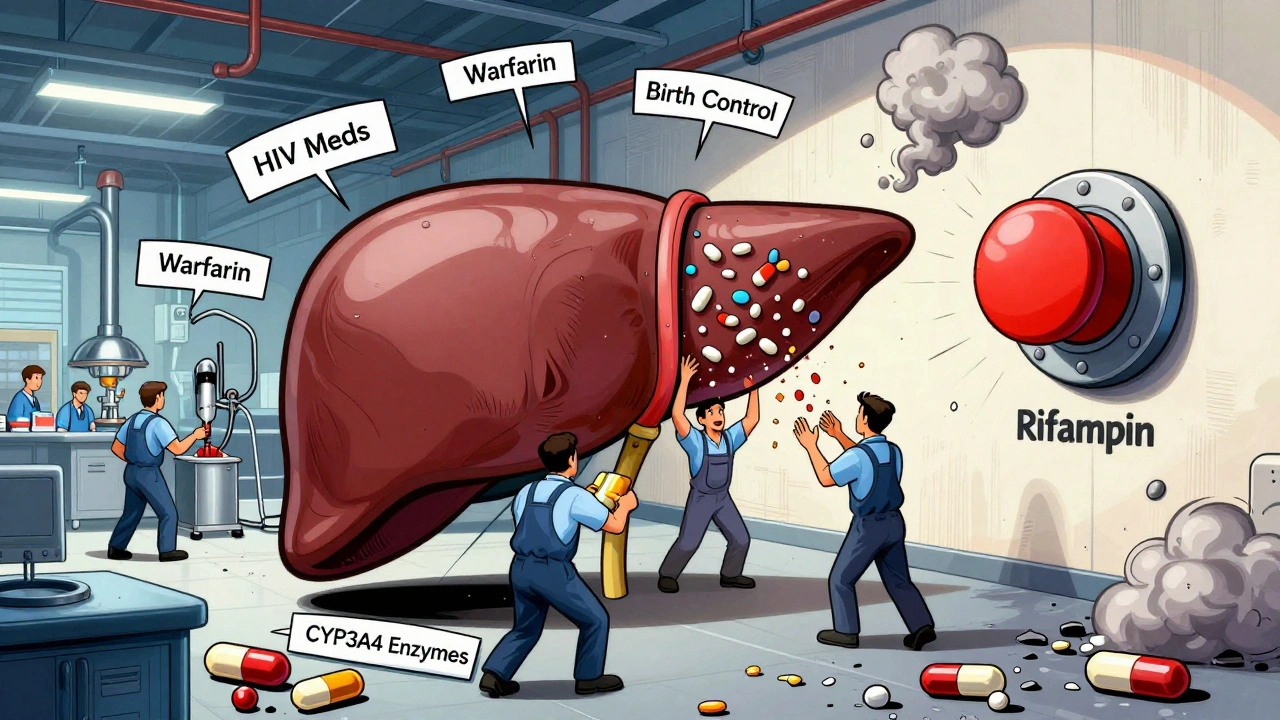
Rifampin, first used in the 1960s, slashed TB treatment from 18 months to six. That’s a 66% reduction in time, saving millions of lives. But its power comes with a cost. Rifampin activates a master switch in your liver called the pregnane X receptor (PXR). Once flipped, this switch turns on a cascade of enzymes-especially CYP3A4-that break down drugs faster than normal. Within 24 hours of your first dose, your body starts treating other medications like they’re trash.
How Rifampin Turns Your Liver Into a Drug-Destroying Machine
Imagine your liver as a factory that processes every pill, supplement, or hormone you take. Normally, it works at a steady pace. Rifampin doesn’t just speed it up-it turns the factory into a demolition crew.
Within three days of taking a standard 600 mg dose, CYP3A4 enzyme activity can jump by 200% to 400%. That means drugs metabolized by this enzyme disappear from your bloodstream before they can do their job. Oral contraceptives? Their effectiveness drops by 67%. Warfarin? Blood thinning drops by 42%, raising your risk of clots. HIV drugs like protease inhibitors? Levels plunge by 75% to 90%. That’s not just a warning-it’s a treatment failure waiting to happen.
And it’s not just the liver. Rifampin also cranks up p-glycoprotein, a transporter that shoves drugs out of cells before they can be absorbed. This hits drugs like digoxin, cyclosporine, and even some cancer meds. A patient on warfarin who starts rifampin might need a 50% dose increase just to stay in range. Stop rifampin? The enzyme levels don’t drop right away. They linger for up to two weeks. That means if you switch from TB meds to a new drug too soon, you’re still at risk of overdose.
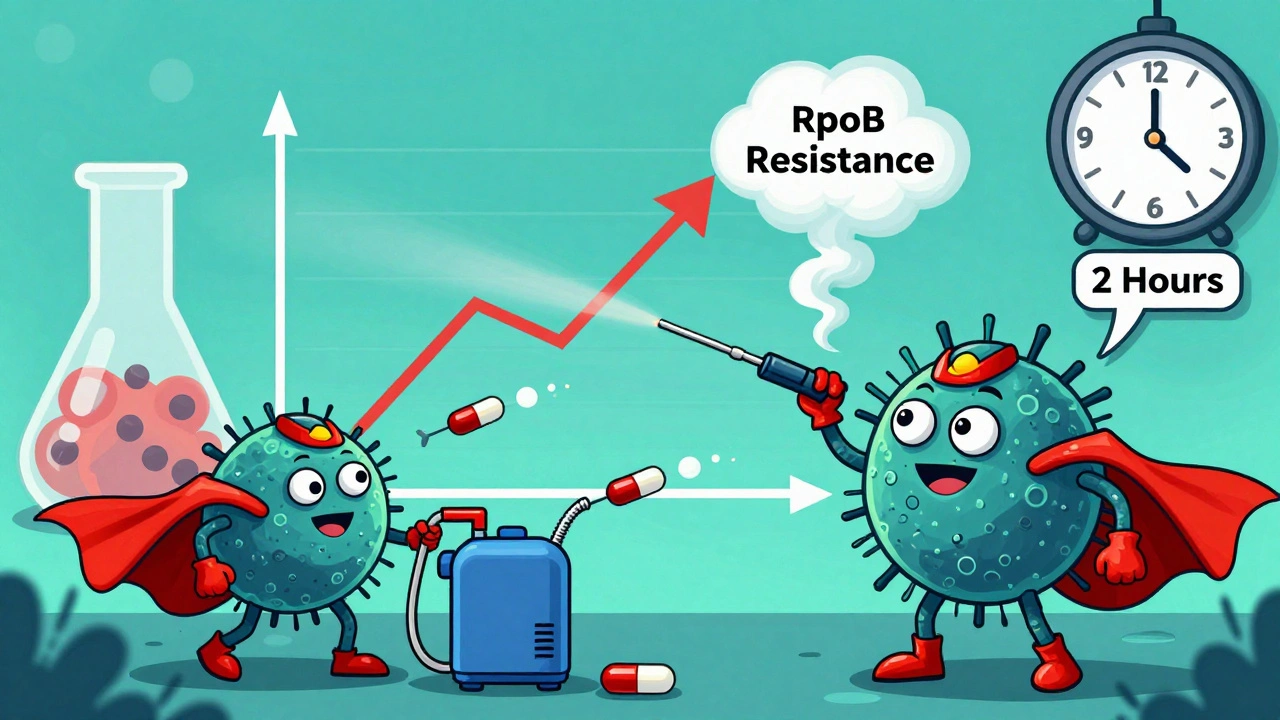
The Paradox: Rifampin Makes TB Bacteria Stronger
Here’s the twist no one talks about: rifampin doesn’t just affect your body-it affects the bacteria it’s supposed to kill.
Research shows that within hours of exposure, even at low doses, rifampin triggers a survival response in *Mycobacterium tuberculosis*. The bacteria start pumping the drug out using special protein pumps. They also ramp up production of a key enzyme called RpoB, which helps them resist the drug’s effects. In lab studies, this happens within two hours. This isn’t resistance you can measure with a standard test-it’s a hidden, temporary tolerance that lets a small group of bacteria survive.
That’s why TB treatment can’t be shortened below four months. Even if symptoms disappear, those surviving bacteria can wake up later and cause relapse. Clinical trials show relapse rates jump to over 25% if treatment ends too soon. So rifampin’s own mechanism forces you to take it longer than you’d expect-six full months, no exceptions.
Common Medications That Can Turn Dangerous With Rifampin
Here’s a practical list of drugs that can fail-or cause harm-when taken with rifampin:
- Birth control pills: Risk of unintended pregnancy. Backup contraception is mandatory.
- Warfarin: INR drops fast. Frequent blood tests needed. Dose adjustments often exceed 50%.
- HIV antivirals: Protease inhibitors (e.g., ritonavir, darunavir) and NNRTIs (e.g., efavirenz) lose effectiveness. Some combinations are outright contraindicated.
- Statins: Atorvastatin and simvastatin levels drop sharply. Rosuvastatin is safer but still monitored.
- Immunosuppressants: Cyclosporine and tacrolimus levels crash. Transplant rejection risk spikes.
- Antifungals: Fluconazole and itraconazole become ineffective.
- Antidepressants: SSRIs like sertraline and citalopram may need higher doses.
- Opioids: Methadone and buprenorphine levels drop, risking withdrawal or relapse.
Even over-the-counter stuff matters. St. John’s wort? It’s a CYP3A4 inducer too. Taking it with rifampin? Double the effect. Herbal supplements are not safe just because they’re natural.
What Doctors Do to Manage These Interactions
Good TB care isn’t just about prescribing rifampin-it’s about auditing every other medication a patient takes.
Before starting TB treatment, a full medication review is non-negotiable. Pharmacists often run interaction checks across all prescriptions, supplements, and even OTCs. If a patient is on warfarin, they’re switched to low-molecular-weight heparin during rifampin therapy. Birth control users get an IUD or barrier method. HIV patients are moved to rifabutin, a weaker inducer that still works against TB.
Timing matters. If you need to start a new drug after rifampin-say, a transplant medication-you wait at least two weeks. For drugs with a narrow safety window, like cyclosporine, you wait four weeks. And when you stop rifampin, you don’t go back to your old dose right away. You start low and titrate up slowly, watching for toxicity.

New Hope: Blocking Rifampin’s Dark Side
What if you could keep rifampin’s power but shut off its side effects? Researchers are trying.
Studies show that common stomach drugs-proton pump inhibitors (PPIs) like omeprazole-can block the bacterial efflux pumps that let TB survive rifampin. In lab tests, omeprazole at normal doses reduced bacterial drug pumping by 68%. That’s huge. If this works in humans, it could mean cutting TB treatment from six months to three.
Another candidate? Verapamil, a heart medication. At low doses, it also blocks those same pumps. Clinical trials are now testing whether adding verapamil or omeprazole to standard TB therapy can lower relapse rates from 25% to under 5%. Early animal results are promising. If this pans out, it won’t just shorten treatment-it could make rifampin safer for millions who need other medications.
What Patients Need to Know Right Now
If you’re on rifampin:
- Never start, stop, or change any medication without telling your TB doctor.
- Carry a list of all your drugs-prescription, OTC, supplements, herbs.
- If you’re on birth control, use condoms or an IUD. Don’t rely on pills.
- Watch for signs of overdose if you stop rifampin: dizziness, nausea, unusual bleeding, confusion.
- Report any new symptoms: yellow skin, dark urine, severe fatigue-these could mean liver damage.
Rifampin is not a drug you take lightly. It’s one of the most effective TB tools we have-but it’s also one of the most dangerous if ignored. Your survival depends on understanding its full impact.
When Liver Damage Happens-and What to Do
Rifampin doesn’t just interfere with other drugs. It can hurt your liver directly. About 1 in 5 people on TB treatment show signs of liver injury: ALT levels more than three times the normal upper limit. Symptoms include nausea, loss of appetite, jaundice, and dark urine.
Doctors monitor liver enzymes monthly during treatment. If levels spike, rifampin may be paused or replaced with another drug like rifabutin. But here’s the catch: even if your liver looks fine, the drug is still changing how your body handles everything else. So liver safety doesn’t mean interaction safety.
And yes, there’s a weird upside: rifampin is sometimes used off-label to treat severe itching in liver disease. It works by boosting bile acid breakdown-cutting ileal reabsorption by 40%. But that’s a controlled hospital use, not something you should try on your own.
Can I take birth control while on rifampin?
No, oral contraceptives become significantly less effective-by up to 67%-when taken with rifampin. You must use a non-hormonal method like an IUD, condoms, or a diaphragm during treatment and for at least two weeks after stopping rifampin. Relying on birth control pills alone risks unintended pregnancy.
How long does rifampin’s effect last after I stop taking it?
The enzyme-inducing effects of rifampin can persist for up to two weeks after your last dose. For drugs with a narrow therapeutic window-like warfarin, cyclosporine, or certain antivirals-doctors recommend waiting four weeks before restarting them to avoid toxicity from suddenly increased drug levels.
Is rifabutin a safer alternative to rifampin?
Yes, for patients on HIV medications or other drugs sensitive to CYP3A4 induction, rifabutin is often preferred. It’s a weaker inducer, meaning it causes fewer interactions. However, it’s more expensive and not always available. It’s also not used as a first-line TB drug unless interactions are a major concern.
Can I drink alcohol while taking rifampin?
It’s best to avoid alcohol. Both rifampin and alcohol are processed by the liver, and combining them increases the risk of liver damage. Even moderate drinking can push enzyme levels into dangerous territory. If you drink regularly, your doctor may need to adjust your treatment plan.
Are there any new treatments that can replace rifampin?
Not yet. Rifampin remains the most effective drug for shortening TB treatment. New drugs like bedaquiline and pretomanid are used for drug-resistant TB, but they don’t replace rifampin in standard cases. Research is ongoing into adding drugs like omeprazole or verapamil to boost rifampin’s effect and shorten treatment-but these are still experimental.

Rifampin is wild. I had a friend on it for TB and she didn't realize her birth control was useless until she got pregnant. No one warned her. Like, why isn't this on every prescription label? It's not just a drug-it's a whole-system reset.
The PXR-CYP3A4 axis is the real villain here. Rifampin’s induction kinetics are textbook-rapid onset, slow offset. But what’s rarely discussed is the pharmacodynamic lag in downstream metabolites. Even when plasma concentrations appear stable, the hepatic clearance profile is fundamentally altered. This isn't just drug interaction-it's metabolic reprogramming. Clinicians need to treat this like a transplant-level interaction, not a footnote.
Thank you for writing this. 💙 I’m a nurse and I’ve seen too many patients get burned by this. One lady on warfarin had a stroke because her INR dropped and no one told her rifampin was the culprit. Please, if you're on this med-keep a meds list. Tell EVERY provider. It’s not just your doctor-it’s your dentist, your physical therapist, your pharmacist. Everyone.
wait so st. johns wort + rifampin = double trouble?? 😳 i had no idea herbal stuff could do this. my aunt takes it for anxiety and just started tb meds. gonna call her right now.
I’m so glad someone finally explained why my cousin had to wait 4 weeks after finishing TB meds before restarting her transplant meds. I thought it was just bureaucracy. Turns out it’s science. This post saved me from making a huge mistake. Thank you.
In India, rifampin is given like candy. People take it for coughs, colds, even acne. No one checks interactions. I’ve seen patients on statins crash their liver because they were on rifampin for a fake TB diagnosis. This needs to be in school curriculums, not just medical journals.
So let me get this straight. A drug that saves millions also makes your birth control useless, your heart meds useless, and your liver hate you? And we call this 'standard of care'? What a joke. Pharma didn't fix this because they profit more from people needing new drugs after the old ones fail.
OMG I just realized my mom is on this and she’s also on lisinopril and a statin 😭 I’m so scared. I’m printing this out and taking it to her doctor tomorrow. You’re a lifesaver for writing this.
My sister is on rifampin right now and she’s terrified. She’s a single mom and was on antidepressants. They had to switch her to a different one and she’s been crying nonstop. This isn’t just about chemistry-it’s about people losing their stability. We need better support systems.
THIS. IS. A. GAME. CHANGER. 🚨 I’ve been researching this for months and no one talks about the bacterial efflux pump thing. The fact that TB bacteria start resisting it within TWO HOURS? That’s terrifying. And omeprazole helping? That’s the kind of hack we need-cheap, available, life-saving. Why isn’t this protocol yet??
They’re hiding this. Always. Rifampin? It’s not just a drug-it’s a bioweapon disguised as medicine. The CDC knows this. The WHO knows this. They let it fly because they don’t care about the 10% who get screwed. They want the numbers to look good. Wake up people. This is control. This is control.
As a pharmacist, I’ve seen this too many times. The real tragedy? Patients think ‘I’m done with TB’ and stop monitoring. But the enzyme levels hang around for weeks. I always give patients a printed timeline: ‘Stop rifampin → wait 14 days → monitor → titrate slowly.’ If you don’t do this, you’re playing Russian roulette with your liver and your heart. This isn’t fear-mongering. It’s protocol.