Getting vaccinated while on immunosuppressants isn’t just about picking a date-it’s about timing. If you’re taking drugs like rituximab, methotrexate, or TNF inhibitors, your immune system is already working under heavy constraints. A vaccine given at the wrong time might not work at all. Too early, and your body hasn’t had time to respond. Too late, and the medication is already suppressing your immune response. The difference between protection and vulnerability often comes down to days, not weeks.
Why Timing Matters More Than You Think
Most people assume vaccines work the same way regardless of what else they’re taking. That’s not true for those on immunosuppressants. These drugs-used for autoimmune diseases, cancer, and organ transplants-dampen the immune system to stop it from attacking the body. But that same suppression can block the vaccine’s ability to trigger protective antibodies. Studies show patients on certain immunosuppressants can have up to 70% lower antibody responses compared to healthy individuals. That’s not a small drop. It’s the difference between being protected and being at risk. The goal isn’t to stop your medication. It’s to find the sweet spot where your immune system has a chance to react to the vaccine before the drug shuts it down. This requires knowing exactly which drug you’re on, how it works, and when it peaks in your system.What the Guidelines Actually Say (And Where They Conflict)
There’s no single rule. Different medical groups have different recommendations, and that creates real confusion for patients and doctors alike. The CDC says: Get vaccinated at least 14 days before starting immunosuppressants. Simple. But that’s the bare minimum. Other groups push for more caution. The American College of Rheumatology (ACR) gives detailed advice based on the drug:- Methotrexate: Hold for two weeks after flu vaccine if your disease is stable. This one’s backed by solid data-three trials showed a 27% increase in antibody response when paused.
- Rituximab: Wait at least six months after your last dose before getting any non-flu vaccine. Why? Rituximab wipes out B-cells, the immune cells that make antibodies. It can take months for them to come back.
- TNF inhibitors (like Humira or Enbrel): Skip one dose before vaccination, then wait four weeks after to restart.
- IVIG: If you’re on high doses (2 grams per kilogram), you need to wait 11 months before a live vaccine and four weeks after.
Real-World Consequences of Getting It Wrong
This isn’t theoretical. People are getting sick because the timing was off. At Massachusetts General Hospital, 42% of patients on rituximab had to wait six months for their shingles vaccine. During that time, 18% ended up with shingles anyway. One patient wrote on a patient forum: “I waited six months. Got shingles anyway. My doctor said it was unavoidable. But I felt like I was left unprotected.” On the flip side, patients who timed it right report better outcomes. One person on a cancer forum said: “My oncologist scheduled my flu shot three weeks before chemo. I haven’t had the flu in three years-even with low white blood cell counts.” The problem isn’t just vaccines. It’s the ripple effect. If you delay a vaccine because your medication hasn’t cleared, you’re exposed longer. If you vaccinate too soon after stopping a drug, your immune system might not be ready. And if you hold your medication to get a vaccine, you risk a flare-up. Cleveland Clinic data shows 31% of patients on hold experienced disease flares. That’s a real trade-off: protect yourself from infection, or risk worsening your underlying condition.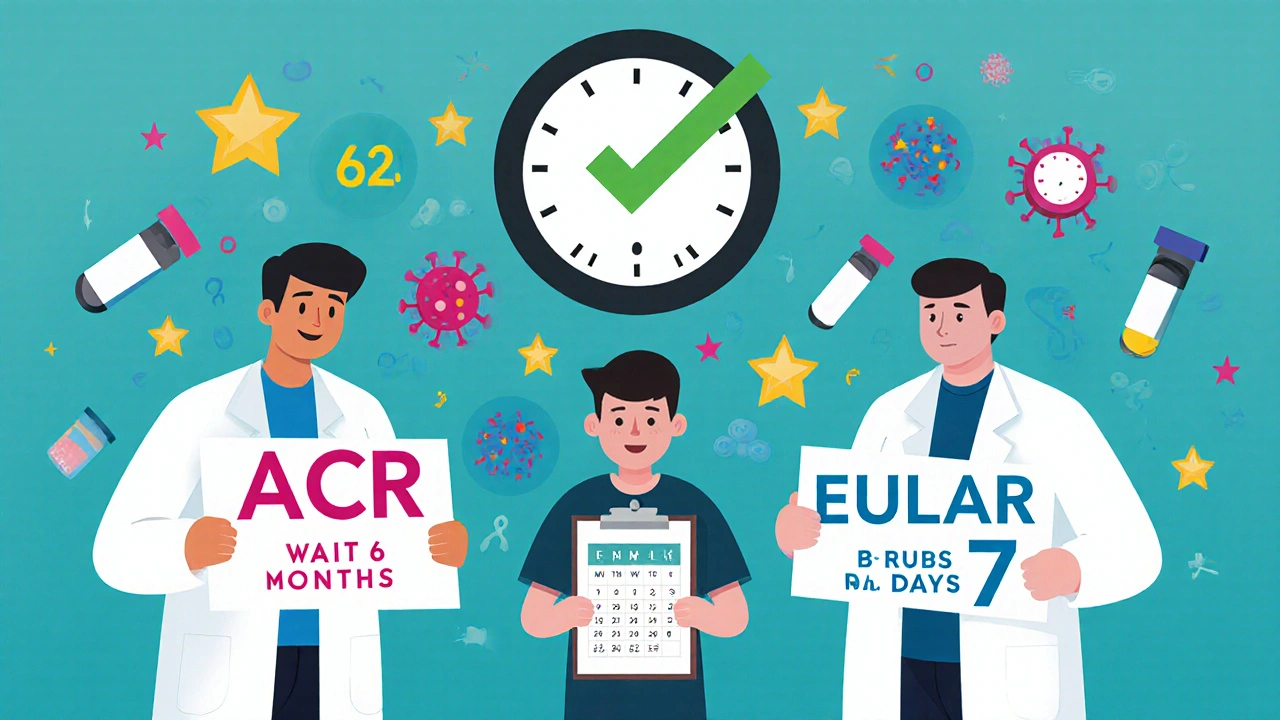
What to Do With Different Medications
Here’s what works based on current evidence:For Rituximab and Other B-Cell Depleters
This is the toughest one. Rituximab, ocrelizumab, ofatumumab-they all clear B-cells. No B-cells, no antibodies. Vaccines won’t stick.- Get all non-live vaccines at least 6 months before your next rituximab dose.
- If you’re already on it, wait at least 6 months after your last infusion before getting vaccines like shingles, pneumococcal, or COVID boosters.
- Flu vaccine is an exception: some experts say it’s okay after 4 months, but only if you’re in a high-risk area.
- Ask for a B-cell count test. If it’s above 50 cells/μL, vaccination may be safe even if it’s been less than 6 months.
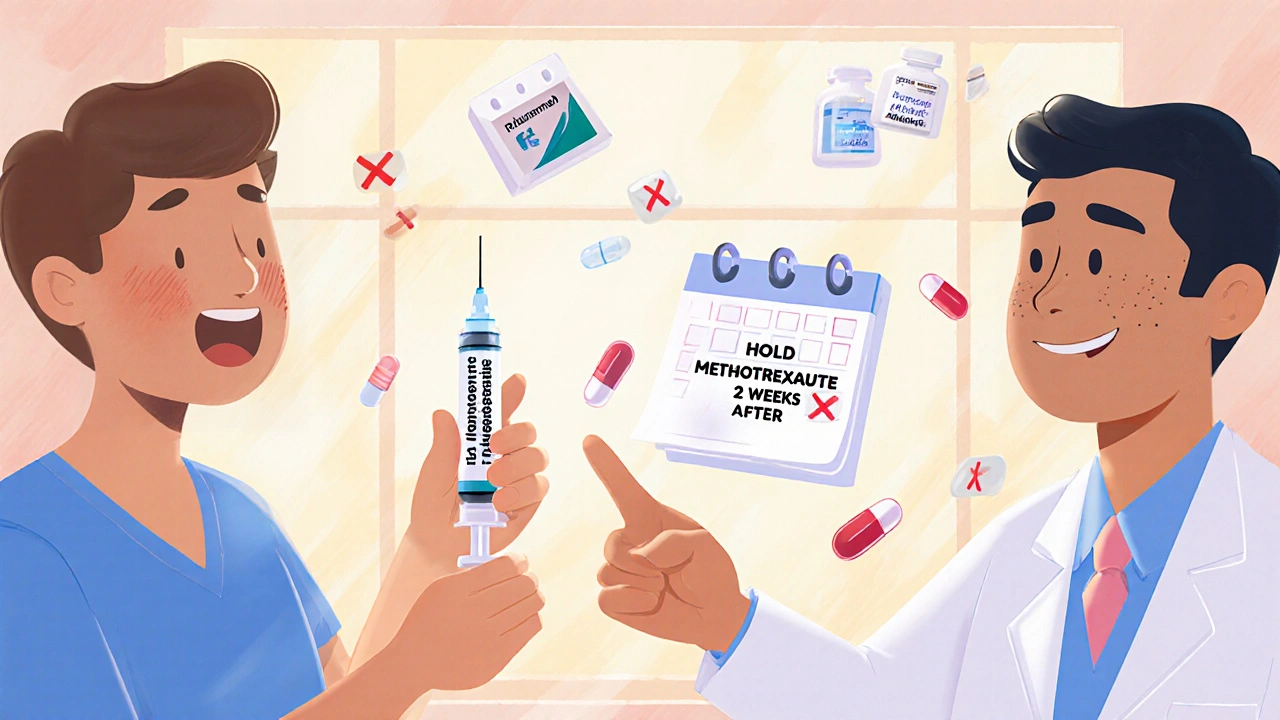
For Methotrexate
This is one of the few cases where a simple pause makes a measurable difference.- Hold methotrexate for two weeks after your flu shot.
- You don’t need to pause for other vaccines unless your doctor says so.
- Don’t stop it for COVID vaccines unless you’re on high doses and your rheumatologist advises it.
For TNF Inhibitors (Humira, Enbrel, Cimzia, etc.)
- Hold one dose before vaccination.
- Wait four weeks after the shot before restarting.
- This applies to all TNF blockers, even if you’re on weekly or biweekly doses.
For Other Immunosuppressants
- Azathioprine, mycophenolate, cyclophosphamide, leflunomide: You can usually keep taking these for non-live vaccines. But stop them 4 weeks before and after live vaccines (like MMR or nasal flu spray).
- Abatacept: No clear benefit to pausing. Vaccines just don’t work as well on this one, regardless of timing.
- IVIG: High doses block vaccine response for months. Check your dose. 1 gram/kg? Wait 10 months before live vaccines.
What About Live Vaccines?
Live vaccines-like MMR, varicella (chickenpox), and the nasal flu spray-contain weakened viruses. In healthy people, they’re safe. In immunosuppressed patients, they can cause infection.- Never get a live vaccine while on immunosuppressants.
- If you need one (like MMR for adults who missed it as kids), get it at least 4 weeks before starting any immunosuppressant.
- If you’re already on meds, you’re out of luck. No exceptions.
- Ask your doctor about alternatives. There’s a shot version of the flu vaccine (inactivated) that’s safe. Same with pneumococcal vaccines.
The Future: Personalized Timing Is Coming
The current guidelines are based on averages. But your body isn’t average. The NIH is running a study called VAXIMMUNE, tracking 2,500 patients to see if measuring immune markers-like B-cell counts, T-cell function, or antibody levels-can predict the best time to vaccinate. Early results suggest fixed time windows might be outdated. Epic Systems, the big EHR company, is building a tool that will automatically calculate your vaccine window based on your meds, dosage, and last treatment date. It’s coming in 2025. That means your doctor’s computer could pop up: “Your rituximab was 7 months ago. B-cell count is 62. Recommended: Get shingles vaccine this week.” For now, the best tool you have is a printed schedule. Write down every drug you take, the last dose date, and the vaccine you need. Bring it to every appointment. Don’t assume your rheumatologist remembers your oncology history. Don’t assume your pharmacist knows you’re on methotrexate.
What You Can Do Today
You don’t need to wait for perfect guidelines. Here’s what to do right now:- Make a list of every immunosuppressant you take, including dose and last date taken.
- Check which vaccines you’re due for: flu, COVID, shingles, pneumococcal, hepatitis B.
- Match your meds to the ACR or IDSA tables above.
- Call your specialist’s office. Ask: “Based on my meds, when’s the safest time to get my next vaccine?”
- Ask if they’ll check your B-cell count if you’re on rituximab.
- Don’t wait for your annual checkup. Schedule a vaccine consult.
When to Push Back
Some doctors stick to rigid timelines because it’s easier. But you have the right to ask for better. If your doctor says, “Just wait six months,” and you’re on rituximab but your B-cell count is normal, ask: “Can we check my immune markers before deciding?” If they say, “We can’t pause your meds,” but you’re on methotrexate and it’s flu season, say: “I’ve read that pausing for two weeks after the shot improves response. Can we try that?” You’re not being difficult. You’re being informed.Final Thought: It’s Not About Perfection. It’s About Protection.
No timing is perfect. Sometimes you’ll have to wait. Sometimes you’ll get sick anyway. But if you get the timing right, you stack the odds in your favor. A vaccine that works might mean the difference between a mild cold and a hospital stay. Between staying home and needing ICU care. The science is clear. The guidelines are messy. But you’re not powerless. With the right info, the right questions, and the right timing-you can protect yourself, even when your immune system is on hold.Can I get the flu shot while on methotrexate?
Yes, you can get the flu shot while on methotrexate. But to improve your immune response, the American College of Rheumatology recommends pausing methotrexate for two weeks after the shot-only if your disease is stable. Studies show this boosts antibody production by 27%. Don’t stop your methotrexate for other vaccines unless your doctor advises it.
How long after rituximab should I wait for a shingles vaccine?
Wait at least six months after your last rituximab infusion before getting the shingles vaccine (Shingrix). Rituximab wipes out B-cells, which are needed to respond to vaccines. Even if you feel fine, your immune system may still be too weak to respond. Some experts recommend checking your B-cell count-if it’s above 50 cells/μL, vaccination may be safe sooner. Always confirm with your rheumatologist.
Can I get a COVID booster while on immunosuppressants?
Yes, and you should. People on immunosuppressants are at higher risk for severe COVID. The CDC and IDSA recommend getting boosters, ideally 14 days before starting a new immunosuppressant or at least 3 months after finishing B-cell depleting drugs like rituximab. If you’re on methotrexate, you can get the booster without pausing. For TNF inhibitors, skip one dose before and wait four weeks after.
Is it safe to get live vaccines like MMR while on immunosuppressants?
No. Live vaccines (MMR, varicella, nasal flu spray) contain weakened viruses that can cause infection in people with suppressed immune systems. Never get these while on immunosuppressants. If you need them, get them at least 4 weeks before starting any immunosuppressive therapy. If you’re already on meds, you’ll need to rely on inactivated alternatives like the shot version of the flu vaccine.
What if I missed the ideal timing for a vaccine?
Don’t panic. It’s better to get the vaccine late than not at all. While your response might be weaker, some protection is still better than none. Talk to your doctor about getting an antibody test after vaccination to see if you developed immunity. If not, you may need a second dose or a different vaccine strategy. New guidelines are moving toward checking immune markers, not just waiting fixed time periods.
Can my primary care doctor handle vaccine timing, or do I need a specialist?
Primary care doctors can help with routine vaccines, but immunosuppressant timing is complex. Most don’t know the nuances between methotrexate, rituximab, and IVIG. Always consult your rheumatologist, oncologist, or transplant specialist before scheduling. Bring your medication list. Use tools like the UCSF Immunossuppressant-Vaccine Timing Calculator to prepare. Coordination between specialists is key-don’t assume everyone’s on the same page.

Just got my flu shot last week. Held methotrexate for two weeks after as advised. Felt fine. No flare. No sickness. Small win.
Worth the hassle.
This is one of those posts that should be printed and laminated. So many people are flying blind with their vaccine timing, and it’s not just about convenience-it’s about survival.
Thank you for laying out the nuances so clearly. I’m sharing this with my rheumatology group tomorrow.
Ugh. I just got the shingles shot. Six months after my last rituximab. Still got shingles. So much for all this ‘perfect timing’ nonsense.
My doctor just shrugged. I’m done listening.
Everyone’s acting like this is rocket science when it’s just basic immunology
Of course your body can’t respond when you’re suppressing it
Why do we need guidelines for common sense
And why do patients think they deserve a perfect outcome when they’re on drugs that literally break their immune system
Stop pretending this is fair
It’s not
It’s just biology
I’ve been living with lupus for 17 years, and I’ve watched the vaccine guidance evolve from ‘don’t get anything’ to ‘here’s a 12-page chart with asterisks’
It’s exhausting, honestly
There’s a quiet grief in being told you’re too fragile for the very things that keep others safe
And yet, we keep showing up, bringing our lists, asking the questions, holding our meds, waiting six months, checking our B-cells, hoping the next dose will stick
It’s not just medical-it’s emotional labor
And somehow, we still manage to be grateful when it works
That’s the real miracle here
Not the science
But us
For those on mycophenolate-yes you can get the flu shot without stopping
But if you're on high dose and have low WBCs, talk to your doc about timing
I got my pneumococcal shot 3 weeks after my last dose and had zero reaction
Just don't assume it's the same for everyone
And please, get your antibody levels checked if you can
It's not expensive and it gives real answers
The discrepancy between ACR and EULAR guidelines reflects a deeper epistemological tension in clinical immunology: population-based protocols versus individualized immunophenotyping
While the former offers operational clarity, the latter-guided by dynamic biomarkers-is the future
Until then, we’re managing risk through probabilistic heuristics
Which is why I always request B-cell quantification before scheduling non-live vaccines
It’s not just prudence-it’s precision medicine in practice
I’m a transplant recipient from the UK, and I’ve had to navigate this maze for over a decade.
My consultant here said, ‘Wait three months.’ My specialist in Boston said, ‘Six months, no exceptions.’
One of them was wrong.
Or maybe both were right-for different people.
It’s infuriating.
But I’ve learned to carry my med list like a sacred text.
And I never, ever trust a doctor who says ‘just follow the CDC’ without asking what’s in your blood.
We’re not patients.
We’re partners in this.
As someone who mentors newly diagnosed autoimmune patients, I always say: Your health is not a checklist, it’s a conversation
Write down your meds, your dates, your vaccines
Bring it to every appointment
Even if your doctor has your chart
Even if you’ve been coming for years
Because no one remembers everything
And your life is worth the extra effort
And if they roll their eyes?
Find a new doctor
You deserve better
Just got my COVID booster this morning!
Paused my Humira like the guide said-skip one dose before, wait four weeks after.
My nurse even printed me a little calendar with the dates marked 😊
Feels good to be proactive.
And hey-if you’re scared or confused?
You’re not alone.
Keep asking.
Keep showing up.
We’ve got this 💪