Chronic Idiopathic Constipation: Causes, Symptoms, and Treatment Options
When dealing with chronic idiopathic constipation, a long‑lasting difficulty passing stools without an identifiable medical cause. Also known as functional constipation, it often shows up in men who ignore subtle warning signs. Understanding it starts with recognizing related factors such as dietary fiber, the plant‑based carbs that add bulk and moisture to stool (sometimes called roughage), laxatives, pharmaceutical aids that stimulate bowel movements or soften stool and pelvic floor therapy, targeted exercises and biofeedback to improve muscle coordination during defecation. These entities interact in predictable ways, forming the backbone of any effective management plan.
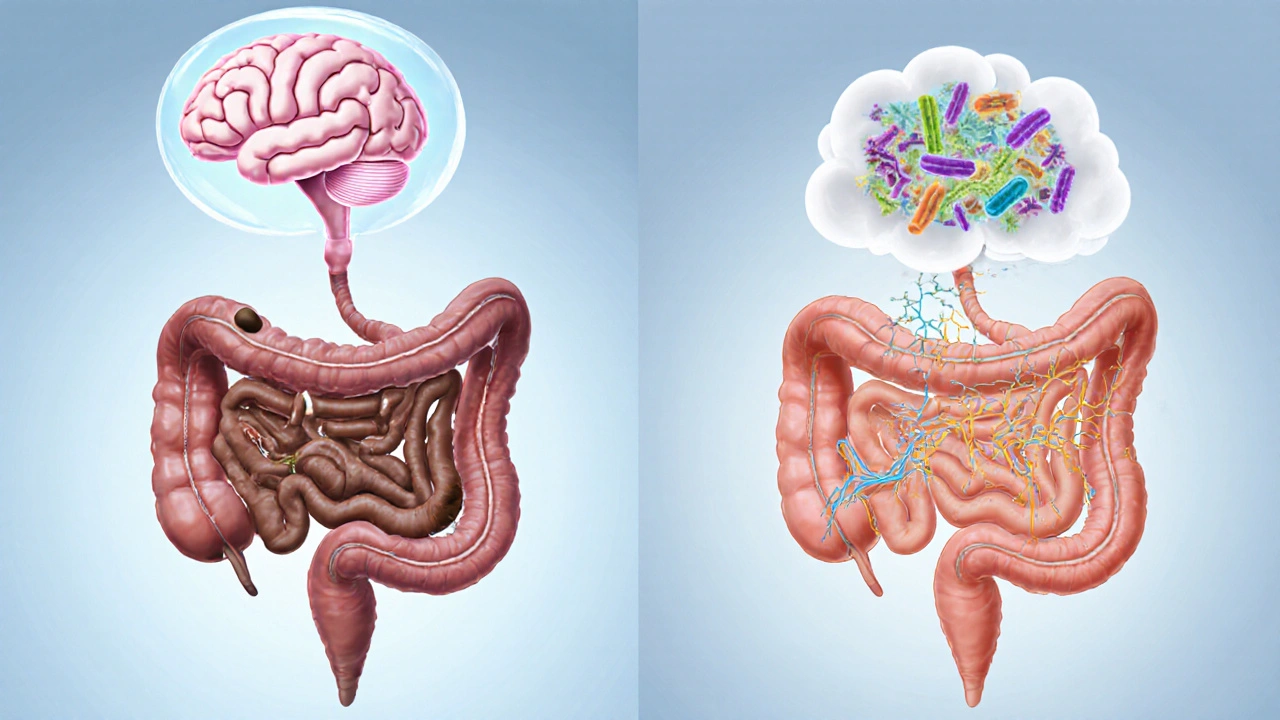
First, chronic idiopathic constipation encompasses persistent bowel‑movement difficulty that lasts for weeks or months, often without an obvious obstruction or disease. The condition demands a multifaceted approach because the root causes can be behavioral (low fiber intake), physiological (slowed colonic transit), or neuromuscular (pelvic floor dysfunction). Studies show that increasing dietary fiber by 10‑15 grams daily can boost stool frequency by 30 % in many patients. Fiber works by absorbing water, expanding in the gut, and prompting peristalsis – the wave‑like muscle contractions that push waste forward.
How Lifestyle, Medication, and Therapy Interact
Effective treatment requires three core steps: modifying diet, using medication when needed, and addressing muscle coordination. Step one tackles the low‑fiber diet that fuels hard, dry stools. Include whole grains, legumes, fruits, and vegetables, or consider a fiber supplement like psyllium if whole foods are hard to digest. Step two introduces laxatives – osmotic agents (e.g., polyethylene glycol) that draw water into the colon, or stimulant laxatives (e.g., bisacodyl) that kick‑start peristalsis. Doctors recommend a short trial of laxatives before moving to stronger options, because long‑term reliance can cause the colon to become lazy.
Step three focuses on pelvic floor therapy. When the pelvic floor muscles contract at the wrong time, stool gets stuck, leading to a cycle of straining and worsening constipation. Biofeedback training helps patients learn to relax the muscles during a bowel movement, improving evacuation efficiency. Many clinics combine this with targeted exercises that strengthen the diaphragm and abdominal muscles, creating a coordinated push that eases passage.
Another piece of the puzzle is hydration. Even with plenty of fiber, insufficient fluids keep stool hard. Aim for at least eight cups of water a day, and avoid excess caffeine or alcohol, which can dehydrate the colon. A simple rule: if your urine is light yellow, you’re probably drinking enough.
Medication side effects can also trigger or worsen constipation. Opioids, certain antidepressants, and anticholinergic drugs slow gut motility. If you’re on any of these, discuss alternatives or adjunct treatments with your doctor. Sometimes a low‑dose peripheral opioid antagonist (like methylnaltrexone) can relieve opioid‑induced constipation without affecting pain relief.
When symptoms persist despite lifestyle tweaks, a doctor may order tests to rule out hidden disorders. Common exams include a colonoscopy, blood work for thyroid function, and a rectal exam to check for structural issues. However, most cases of chronic idiopathic constipation are functional, meaning the gut works fine once the right habits are in place.
To sum up the relationships: chronic idiopathic constipation requires dietary fiber for bulk, laxatives for softening or stimulating stool, and pelvic floor therapy for proper muscle coordination. Each component supports the others – fiber supplies the material, laxatives ensure it moves, and therapy guarantees the muscles don’t stand in the way. Ignoring any one piece can stall progress.
Below you’ll find a curated set of articles that dig deeper into each of these areas. Whether you want quick tips on boosting fiber, a breakdown of safe laxative use, or a step‑by‑step guide to pelvic floor exercises, the collection offers practical insights you can start using right away.