Drug Hypersensitivity: What It Is, How It Happens, and What to Watch For
When your body reacts badly to a medicine you’ve taken before, it’s not just a coincidence—it’s drug hypersensitivity, an immune system overreaction to a medication that isn’t related to its intended effect. Also known as Type B adverse drug reactions, this isn’t about taking too much or taking it wrong—it’s about your body seeing the drug as an invader. Unlike predictable side effects like nausea or drowsiness, drug hypersensitivity can show up days or even weeks after you start a new medicine, and it doesn’t get worse with higher doses. It can hit anyone, even if they’ve used the same drug safely for years.
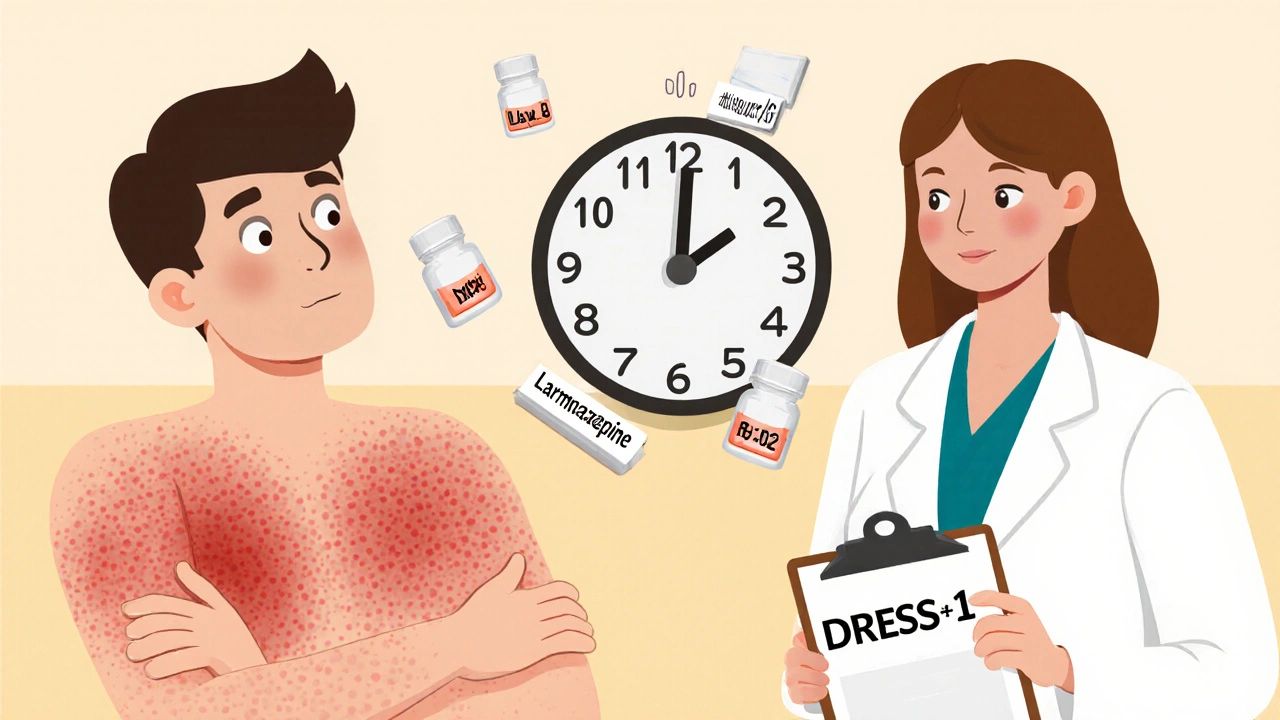
This kind of reaction isn’t rare. Studies show that up to 10% of hospital admissions for drug reactions are linked to hypersensitivity. Common triggers include antibiotics like penicillin, painkillers like NSAIDs, and anticonvulsants like carbamazepine. But it’s not just the drug itself—sometimes it’s a metabolite, a breakdown product your body makes after processing the medicine. That’s why you might react to one brand but not another, or why a reaction might appear suddenly after months of safe use. Type B reactions, unpredictable immune-driven responses to drugs, are the opposite of Type A reactions (like stomach upset from NSAIDs), and they’re harder to spot because they don’t follow a dose-response pattern.
Signs can range from mild—like a skin rash, itching, or hives—to serious, like fever, swollen lymph nodes, or trouble breathing. In rare cases, it leads to conditions like Stevens-Johnson syndrome or toxic epidermal necrolysis, where the skin starts to peel off. If you’ve ever had a bad reaction to a drug, even if it was years ago, that’s important history to share with every doctor. Your immune system remembers. And if you’ve had one hypersensitivity reaction, you’re more likely to have another, especially with drugs in the same class.
That’s why patient-reported outcomes matter. If you notice a new rash after starting a new pill, or if your throat starts swelling after taking a common painkiller, that’s not "just bad luck." It’s data. That feedback helps regulators and doctors spot patterns and warn others. Adverse drug reactions, unexpected harmful effects from medications like hypersensitivity are underreported—many people just stop taking the drug and don’t tell anyone. But when you report it, you help make future prescriptions safer.
What you’ll find in these articles isn’t just theory. You’ll see real cases: how someone developed a rash from an antibiotic they’d used for years, why a diabetes drug caused unexpected skin sensitivity, how photosensitivity from certain meds can look like a sunburn but isn’t, and why some people react to generic versions differently than brand names—even when they’re supposed to be identical. You’ll learn how to track your own reactions, what questions to ask your pharmacist, and how to recognize when a reaction is serious enough to rush to the ER. This isn’t about scaring you—it’s about giving you the tools to speak up before it’s too late.
Delayed drug reactions can appear days or weeks after taking a medication and range from mild rashes to life-threatening conditions like DRESS or Stevens-Johnson Syndrome. Learn the signs, causes, and what to do if you suspect one.