Irritable Bowel Syndrome – What It Is and How to Manage It
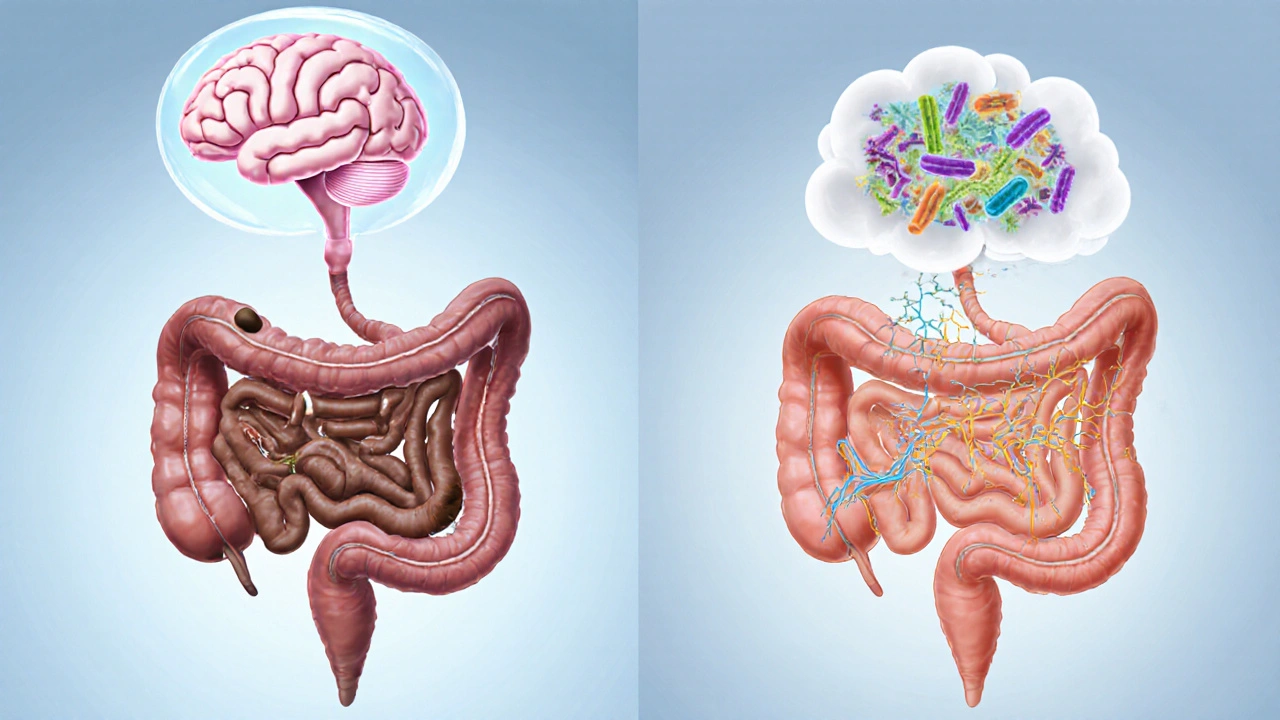
When dealing with Irritable Bowel Syndrome, a common functional gastrointestinal disorder marked by abdominal pain, bloating, and irregular bowel movements. Also known as IBS, it affects millions worldwide and often sparks frustration because symptoms can flare without clear triggers. Understanding IBS starts with recognizing its core components – gut microbiome, the community of bacteria that influences digestion and immune response and dietary fiber, the plant‑based carbohydrate that adds bulk and feeds healthy gut bacteria. irritable bowel syndrome isn’t just a stomach issue; it’s a signal that the brain‑gut axis, stress levels, and lifestyle choices are out of sync.
Managing the condition requires a multi‑step approach. First, diet modification is essential: low‑FODMAP foods reduce fermentable sugars that can trigger gas and pain, while soluble fiber like psyllium helps regularize stool consistency. Second, stress management plays a pivotal role because cortisol spikes can intensify gut motility disturbances; practices such as mindfulness, regular exercise, and adequate sleep often lower symptom frequency. Third, targeted medication provides relief when lifestyle tweaks fall short – antispasmodics ease cramping, laxatives address constipation, and certain low‑dose antidepressants can modulate pain perception. Together, these strategies illustrate how IBS encompasses dietary changes, stress reduction, and pharmacologic support.
Below you’ll find a curated set of articles that dive deeper into each of these areas. From practical tips on choosing the right fiber supplement to reviews of common IBS medications and guidance on stress‑reduction techniques, the collection offers actionable insights for anyone coping with IBS. Explore the resources to build a personalized plan that tackles the root causes and improves daily comfort.
Explore how chronic idiopathic constipation and irritable bowel syndrome are linked, their shared mechanisms, diagnostic tips, and effective treatments in a clear, practical guide.