Stevens-Johnson Syndrome: Causes, Risks, and What You Need to Know
When your body mistakes a medication for an invader, it can trigger something called Stevens-Johnson Syndrome, a severe immune reaction that attacks the skin and mucous membranes. Also known as SJS, this condition starts with flu-like symptoms but quickly turns dangerous—blistering, peeling skin, and painful sores in the mouth, eyes, or genitals. It’s rare, but it’s life-threatening, and it often begins with a drug you thought was harmless.
Most cases are linked to adverse drug reactions, unexpected and harmful responses to medications that aren’t listed as common side effects. Antibiotics like sulfonamides, antiseizure drugs like carbamazepine, and painkillers like naproxen or ibuprofen are frequent culprits. But it’s not just about the drug—it’s about your genes, your immune system, and how your body processes it. Some people have a genetic marker (HLA-B*15:02) that makes them far more likely to react badly. That’s why one person can take the same pill without issue, while another ends up in the hospital.
What makes photosensitivity, an increased skin reaction to UV light caused by certain medications so dangerous here? Many drugs linked to Stevens-Johnson Syndrome also make your skin more sensitive to sunlight. That means even a short walk outside can worsen the reaction. If you’re on a medication that says "may cause sun sensitivity," don’t ignore it. Protecting your skin isn’t just about avoiding sunburn—it could be the difference between a mild rash and a full-blown crisis.
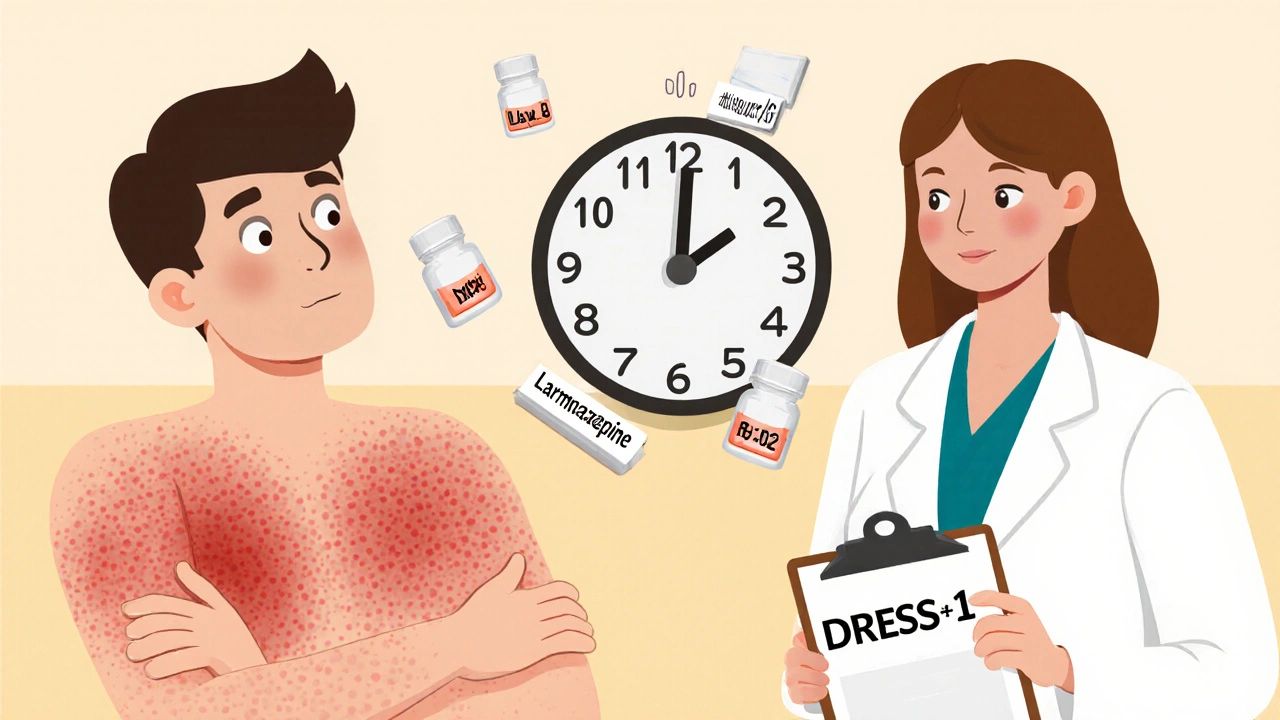
Stevens-Johnson Syndrome doesn’t happen overnight. It usually starts 1 to 3 weeks after starting a new drug. Early signs? Fever, sore throat, burning eyes, or a red, painful rash that spreads fast. If you notice any of these after starting a new medication, stop taking it and get help immediately. Waiting even a day can make things worse.
There’s no cure for SJS—only support. Treatment means stopping the drug, hospital care, wound management, and sometimes intensive care. Recovery can take weeks or months. Some people lose vision. Others have lasting skin damage. That’s why prevention matters more than treatment.
The posts below cover real-world connections you won’t find in most medical guides. You’ll see how drugs like acetazolamide and tetracycline can trigger unusual reactions, why patient feedback helps catch these risks early, and how something as simple as taking a pill with food—or without it—can change your body’s response. You’ll also learn how to spot the difference between a common side effect and a warning sign that demands action. These aren’t theoretical discussions. They’re based on what people have actually experienced, what doctors have seen, and how drug safety systems are trying to catch these reactions before they happen.
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis are rare but deadly drug reactions that cause skin and mucous membrane damage. Learn the warning signs, top triggers, and why genetic testing could save your life.
Delayed drug reactions can appear days or weeks after taking a medication and range from mild rashes to life-threatening conditions like DRESS or Stevens-Johnson Syndrome. Learn the signs, causes, and what to do if you suspect one.