Diabetes and Erectile Dysfunction: What You Need to Know
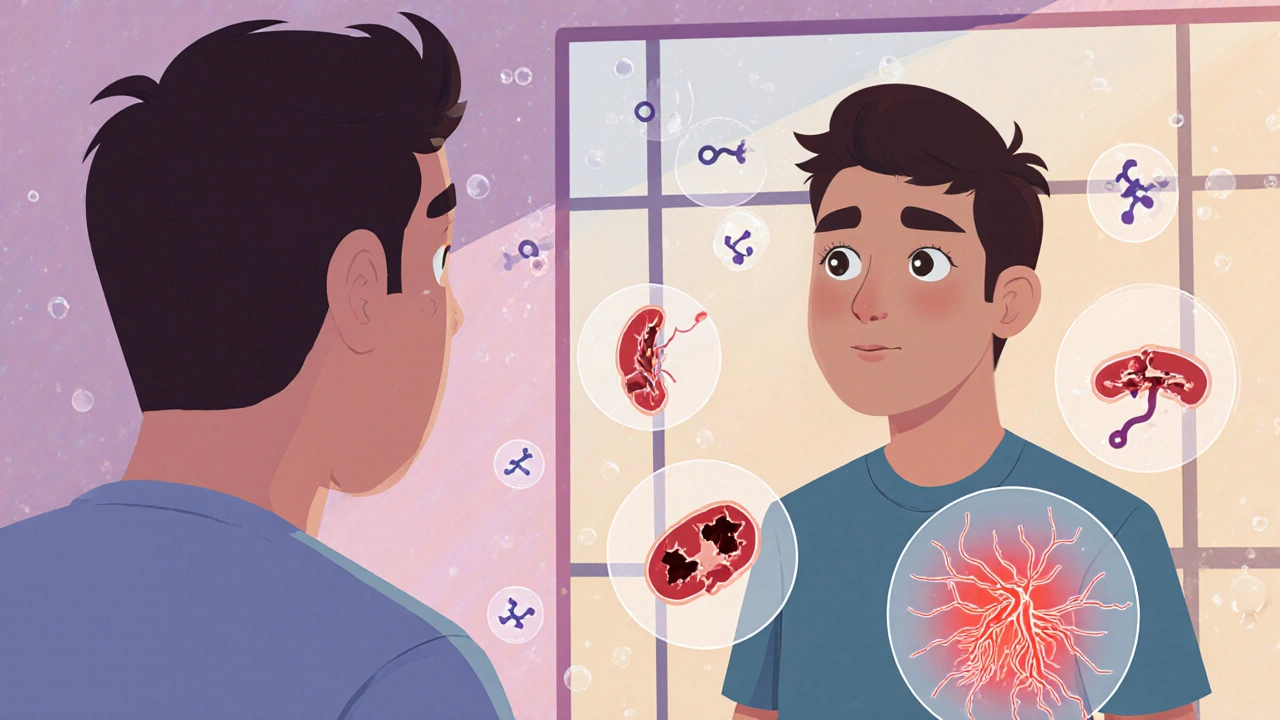
When you have diabetes, a chronic condition where the body can’t properly regulate blood sugar. Also known as type 2 diabetes, it doesn’t just raise your risk for heart disease or kidney problems—it’s one of the leading causes of erectile dysfunction, the inability to get or keep an erection firm enough for sex. This link isn’t random. High blood sugar over time damages blood vessels and nerves, both of which are essential for normal erectile function.
Think of your penis like any other part of your body: it needs good blood flow. Diabetes narrows and hardens the arteries, reducing how much blood can reach the penis during arousal. At the same time, it messes with the nerves that send signals from your brain to your genitals. No signal, no erection—even if you’re turned on. And it’s not just about age or lifestyle. Men with diabetes are three times more likely to have erectile dysfunction than those without it, often years earlier. The worse your blood sugar control, the higher the risk. It’s not a side effect you can ignore—it’s a warning sign your body is under stress.
What makes this even more frustrating is that many men don’t talk about it. They think it’s just part of getting older, or they’re embarrassed to bring it up with their doctor. But here’s the truth: if you have diabetes and you’re having trouble with erections, it’s not your fault. It’s a known medical consequence, and it’s treatable. Medications like PDE5 inhibitors (think Viagra or Cialis) can help, but they won’t fix the root problem. Managing your blood sugar, losing weight if needed, quitting smoking, and staying active can actually reverse some of the damage. It’s not about quick fixes—it’s about long-term health.
Some of the posts here dig into how specific diabetes medications affect sexual health, how other conditions like high blood pressure or depression play into the mix, and what alternatives exist when standard treatments don’t work. You’ll find practical advice on monitoring your symptoms, understanding drug interactions, and making lifestyle changes that actually stick. This isn’t just about sex—it’s about knowing your body, recognizing early signs of decline, and taking action before things get worse. If you’re living with diabetes, this connection matters. And you’re not alone in dealing with it.
Sitagliptin phosphate may help improve erectile dysfunction in men with type 2 diabetes by supporting blood vessel health and lowering blood sugar over time-not as a direct ED treatment, but as a side benefit of better metabolic control.