Erythromycin: What It Is, How It Works, and What You Need to Know
When your body fights a bacterial infection, sometimes you need help—and that’s where erythromycin, a macrolide antibiotic used to treat bacterial infections by stopping bacteria from growing. Also known as a broad-spectrum antibiotic, it’s been around for decades but still plays a key role in treating everything from skin infections to respiratory bugs. Unlike penicillin, it’s often used when someone is allergic to it, making it a go-to alternative for many. But it’s not a cure-all, and using it the wrong way can cause more harm than good.
Erythromycin doesn’t work on viruses, so if you’ve got the flu or a cold, it won’t touch it. But for strep throat, pneumonia, whooping cough, or even acne, it can be effective. It’s also used to prevent infections before surgery or in people with weakened immune systems. What you might not know is that it can interfere with other meds. For example, if you’re taking something for heart rhythm, cholesterol, or even some antidepressants, erythromycin can make their side effects worse. That’s why doctors check your full list of meds before prescribing it. And if you’ve ever had liver problems or a history of long QT syndrome, this drug can be risky.
Side effects are common—stomach upset, nausea, diarrhea, and cramps happen in a lot of people. That’s why some versions are made to be taken with food, even though food can lower how much gets into your system. It’s a balancing act. And while most people finish the course without issue, rare but serious reactions like Stevens-Johnson Syndrome, a dangerous skin reaction triggered by certain drugs, including erythromycin can occur. That’s why you need to watch for rashes, blisters, or mouth sores and call your doctor right away if they show up. Delayed reactions don’t always show up the day you start the pill—they can creep in days or even weeks later, which is why tracking how you feel after starting any new drug matters.
It’s also worth noting that erythromycin isn’t the only antibiotic out there. Alternatives like azithromycin or clarithromycin are often used now because they’re easier on the stomach and taken less often. But erythromycin still has its place, especially in kids, pregnant women, or when other options aren’t suitable. What you need to know isn’t just how to take it—but when to question it. If your symptoms don’t improve after a few days, or if you feel worse, it’s not just a bad day—it could be the infection isn’t responding, or something else is going on.
There’s a reason this drug shows up in so many of the posts here. It’s not just about treating an infection—it’s about understanding how antibiotics interact with your body, your other meds, and your long-term health. From how it affects gut bacteria to why it can mess with your liver enzymes, erythromycin connects to bigger topics like drug safety, side effect timing, and patient-reported outcomes. You’ll find posts here that dig into those links—how it compares to tetracycline, what to do if you miss a dose, and how to spot the warning signs of a bad reaction before it turns dangerous. This isn’t just a drug guide. It’s a crash course in using antibiotics wisely, safely, and with your full awareness.
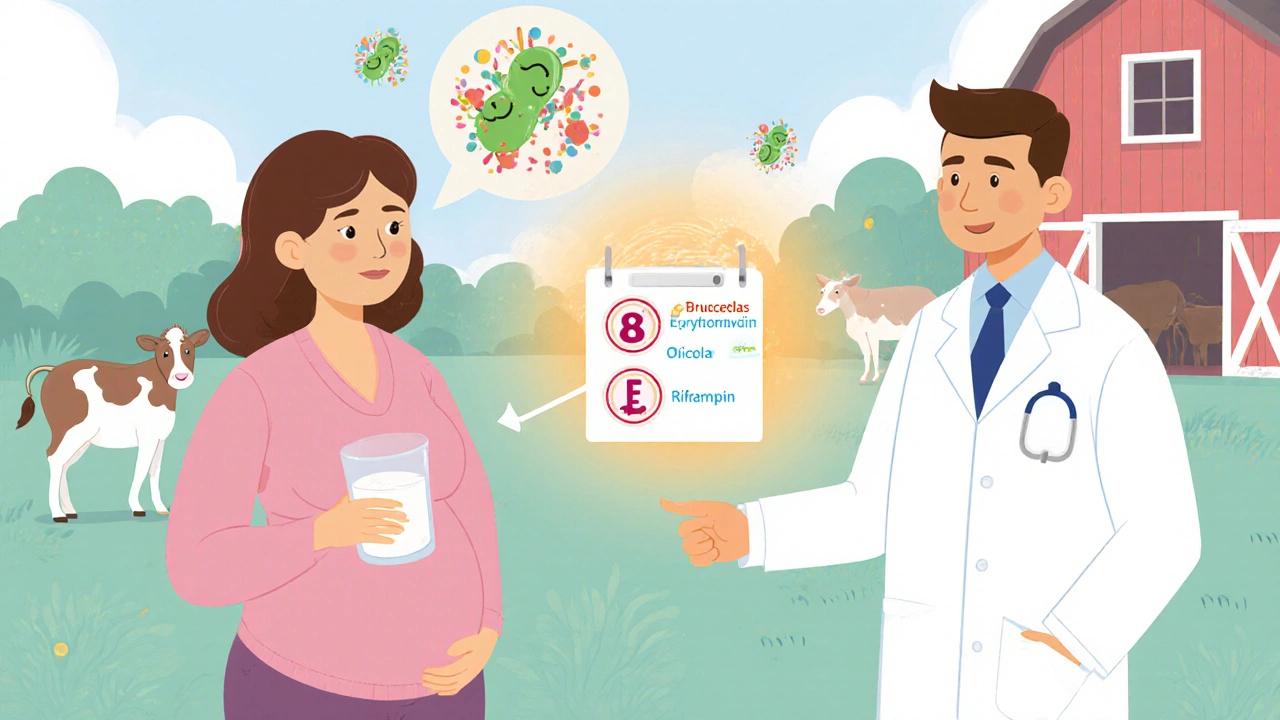
Erythromycin is a key antibiotic for treating brucellosis in pregnant women, children, and those allergic to doxycycline. Learn how it works, proper dosing, side effects, and why it's always used with another drug.