Antiplatelet Therapy
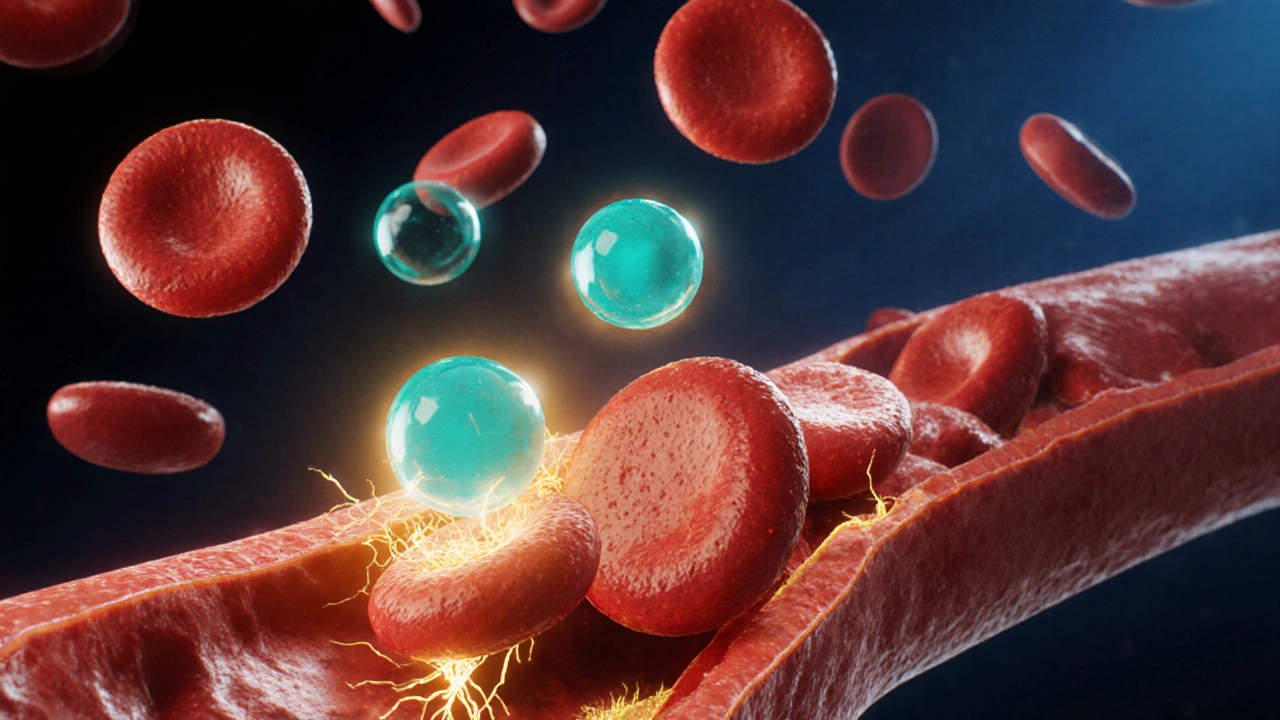
When working with antiplatelet therapy, a treatment that prevents platelets from clumping together to form harmful clots. Also known as antiplatelet drugs, it plays a crucial role in reducing heart attacks, strokes, and other cardiovascular events. Antiplatelet agents are distinct from anticoagulants because they target platelet aggregation rather than the clotting cascade. Two of the most common agents are Aspirin, an irreversible COX‑1 inhibitor that lowers thromboxane A2 production and Clopidogrel, a P2Y12 receptor blocker that stops ADP‑mediated platelet activation. Together, these drugs form the backbone of modern antiplatelet therapy.
Key Antiplatelet Agents and Their Roles
Antiplatelet therapy encompasses several drug classes, each with a specific mechanism. Aspirin’s COX‑1 inhibition reduces platelet stickiness, which is why a low daily dose (often 81 mg) is enough for most patients. Clopidogrel, on the other hand, requires metabolic activation and is frequently prescribed after coronary stent placement to keep the device free of clots. Other agents like ticagrelor and prasugrel act on the same P2Y12 pathway but offer faster onset or stronger platelet inhibition, fitting particular clinical scenarios. The choice of agent depends on the underlying condition—acute coronary syndrome, peripheral artery disease, or primary prevention of stroke—and on patient factors such as bleeding risk, drug interactions, and tolerance.
Using antiplatelet drugs after procedures is a classic example of a semantic triple: antiplatelet therapy enables stent patency. In practice, cardiologists prescribe a dual‑antiplatelet regimen (often aspirin plus clopidogrel) for at least six months post‑stent to minimize re‑occlusion. This regimen illustrates the connection between the drug class and its intended outcome. For patients with atrial fibrillation, clinicians must weigh antiplatelet therapy against full‑strength anticoagulation, because the two approaches target different steps in clot formation.
While antiplatelet drugs are life‑saving, they carry risks. The most common side effect is bleeding, ranging from minor bruising to gastrointestinal hemorrhage. Regular monitoring, especially when combining multiple agents, helps catch early signs of trouble. Patients should avoid non‑steroidal anti‑inflammatory drugs (NSAIDs) that can amplify aspirin’s effect and increase bleeding risk. Lifestyle factors—like limiting alcohol, maintaining a healthy weight, and quitting smoking—also support the benefits of antiplatelet therapy.
In the listings below, you’ll find concise guides on buying common medications safely online, detailed comparisons of antiplatelet options, and practical tips for managing side effects. Whether you’re looking for dosage advice, want to understand how aspirin works, or need to choose the right post‑procedure regimen, the articles ahead give clear, actionable information to help you make informed choices.
A detailed comparison of dipyridamole with aspirin, clopidogrel, ticagrelor and other antiplatelet options, covering mechanisms, side effects, costs, and when each drug is best used.