Rituximab: What It Is, How It Works, and What You Need to Know
When you hear rituximab, a lab-made antibody that targets specific immune cells to treat cancer and autoimmune disorders. Also known as Rituxan, it doesn't work like traditional chemotherapy—it's more like a smart missile that finds and disables harmful B-cells in your body. Unlike vaccines, which train your immune system to fight future threats, rituximab directly shuts down overactive or cancerous immune cells right now. That’s why it’s used for conditions like lymphoma, rheumatoid arthritis, and vasculitis—not to prevent disease, but to stop it in its tracks.
It’s not a one-size-fits-all drug. People with non-Hodgkin’s lymphoma often get rituximab because it zeroes in on CD20 proteins found on cancerous B-cells. In autoimmune diseases like lupus or pemphigus, it reduces the number of cells that mistakenly attack healthy tissue. But it doesn’t touch all immune cells—just the ones that carry CD20. That’s why doctors call it monoclonal antibody, a highly specific protein designed to bind to one exact target on a cell. This precision means fewer side effects than broad immunosuppressants, but it still leaves you vulnerable to infections. That’s why tracking fever, fatigue, or unusual bruising matters.
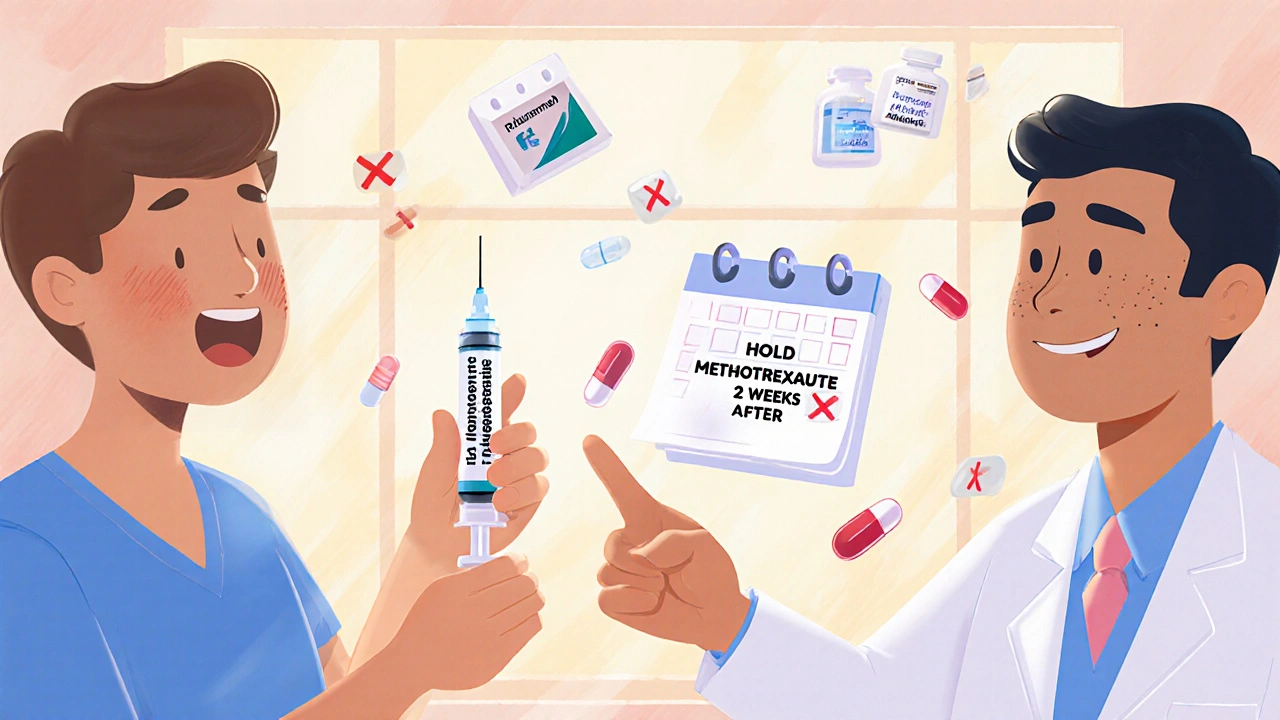
What you won’t find in most brochures is how long it takes to work. Some patients feel better in weeks. Others need months. And because it wipes out B-cells, your body’s ability to respond to new infections drops. That’s why getting a flu shot before starting treatment matters—vaccines won’t work well once you’re on rituximab. It also doesn’t mix well with certain other drugs. If you’re on steroids or other immunosuppressants, your doctor needs to know. There’s no magic pill here—just careful timing, monitoring, and patience.
People often confuse rituximab with vaccines because it’s given as an IV infusion, like some cancer treatments. But it doesn’t trigger immunity. It suppresses it. That’s a big difference. You can’t catch COVID from rituximab, but you might have a harder time fighting it off if you’re exposed. That’s why tracking your health daily—recording symptoms, infections, or reactions—isn’t optional. It’s part of the treatment.
Behind every use of rituximab is a story of balance: fighting disease without leaving the body defenseless. The posts below cover what happens when this drug interacts with other treatments, how side effects show up weeks later, why some patients need repeat doses, and how to spot dangerous reactions before they turn serious. You’ll find real advice from people who’ve been there—on managing fatigue, avoiding infections, understanding lab results, and knowing when to call your doctor. This isn’t theory. It’s what works when your health is on the line.
Timing vaccines correctly while on immunosuppressants is critical for protection. Learn exact guidelines for methotrexate, rituximab, TNF inhibitors, and more-and what to do when the advice conflicts.