AUC Explained: What It Means for Drug Safety and Effectiveness
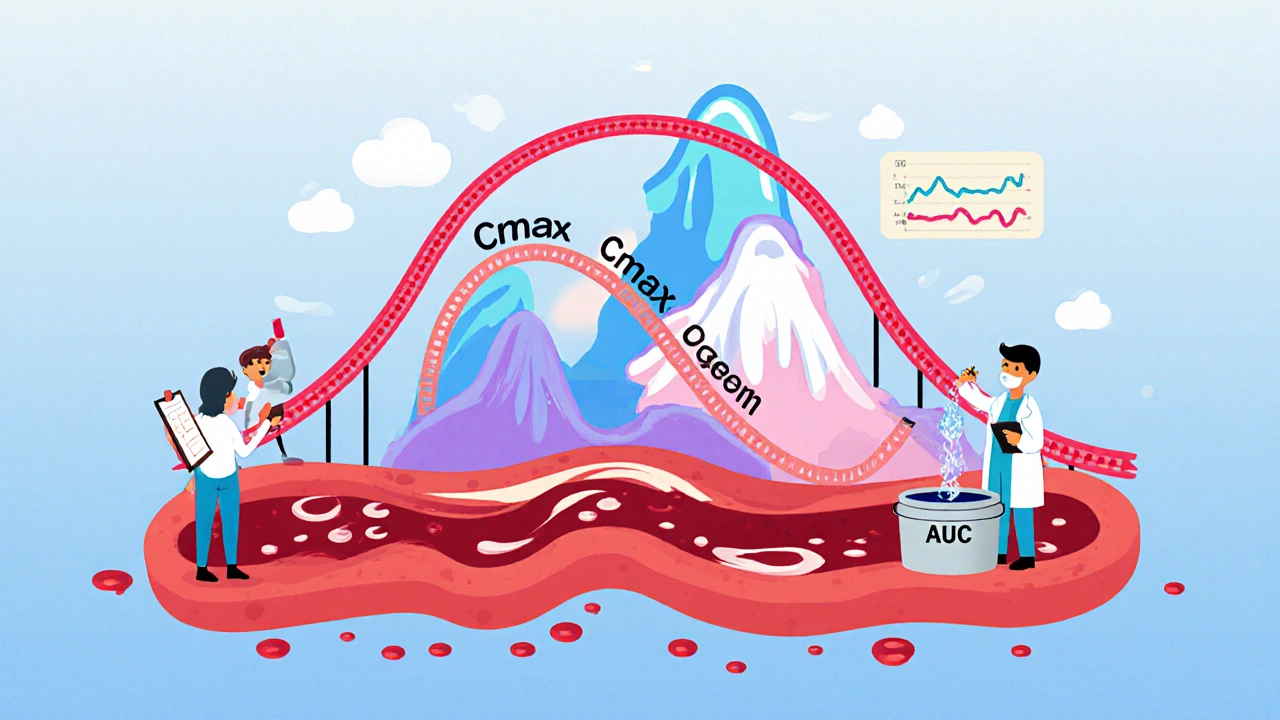
When you take a pill, your body doesn’t just absorb it all at once. AUC, or Area Under the Curve, is a key measure that shows how much of the drug enters your bloodstream and stays there over time. Think of it like tracking how much water fills a bucket over an hour—AUC measures the total amount of medicine your body absorbs, not just the peak. It’s not a number you see on a prescription, but it’s one of the most important factors doctors and researchers use to decide if a drug works safely and consistently.
Bioavailability, how much of a drug actually reaches your system after you take it, directly affects AUC. If a drug is poorly absorbed—say, because you took it with a high-fat meal or your stomach is too acidic—the AUC drops. That means less medicine is doing its job. On the flip side, if your liver breaks it down too fast, AUC falls again. This is why some meds must be taken on an empty stomach, while others need food. Pharmacokinetics, the science of how your body moves drugs through absorption, distribution, metabolism, and elimination is the full picture, and AUC is the heartbeat of that process. It’s also why generic drugs must prove they match brand-name versions in AUC before they’re approved by the FDA.
When AUC is too high, you risk side effects. Too low, and the drug won’t work. That’s why people on long-term meds like entecavir for hepatitis B or sitagliptin for diabetes need regular checkups—doctors track how their body handles the drug over time. AUC helps explain why two people on the same dose can have totally different results. Age, liver function, kidney health, and even gut bacteria can change your AUC. That’s why patient-reported outcomes matter: if you feel off, it might not be the drug—it might be your body’s unique AUC pattern.
Some drugs, like opioids or sertraline, have narrow safety windows. A small change in AUC can mean the difference between relief and danger. That’s why drug interactions—like combining ACE inhibitors with potassium-sparing diuretics—can be risky. They alter how your body processes the medicine, changing AUC without you knowing. Even something as simple as taking a supplement or eating grapefruit can shift AUC enough to cause problems.
Understanding AUC isn’t about memorizing numbers. It’s about knowing why your meds work—or don’t—based on how your body handles them. Whether you’re managing diabetes, depression, or chronic infection, AUC is the silent driver behind dose timing, food rules, and why some people need adjustments while others don’t. Below, you’ll find real-world guides on how drugs behave in your body, what affects their absorption, and how to spot when something’s off.
Cmax and AUC are the two key pharmacokinetic measures used to prove generic drugs are as safe and effective as brand-name versions. Here's how peak concentration and total exposure determine bioequivalence.