CYP3A4 Induction: How It Affects Your Medications and What You Need to Know
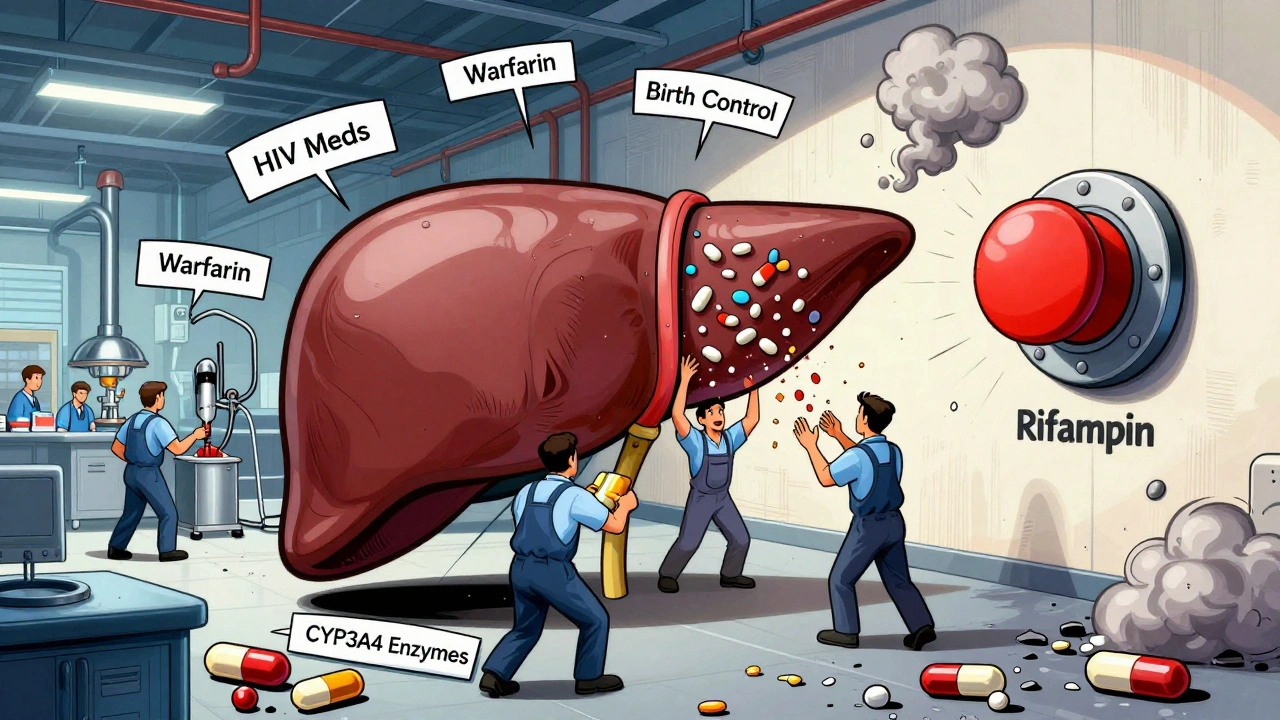
When your body starts producing more of the enzyme CYP3A4, a liver enzyme responsible for breaking down over half of all prescription drugs. Also known as cytochrome P450 3A4, it acts like a molecular factory that processes medications so your body can eliminate them. But when this enzyme gets boosted—called CYP3A4 induction—it can speed up drug breakdown so fast that your meds stop working. This isn’t theoretical. It’s happening right now to people taking common drugs like birth control, statins, or blood pressure pills—without them even realizing it.
What causes CYP3A4 induction? Everyday things: St. John’s wort, some antibiotics like rifampin, even certain seizure meds like carbamazepine. These aren’t rare outliers—they’re widely used. And when they trigger CYP3A4 induction, they don’t just affect one drug. They can slash the effectiveness of dozens. A study in the Journal of Clinical Pharmacology showed that St. John’s wort reduced blood levels of the HIV drug indinavir by up to 57%. That’s not a minor drop—it’s a treatment failure. The same thing happens with birth control pills, immunosuppressants like cyclosporine, and even some cancer drugs. Your doctor might know about this, but if you’re taking supplements or over-the-counter herbs, they might not ask. That’s where the risk hides.
And it’s not just about what you take. It’s about timing. If you start or stop something that induces CYP3A4, the effects don’t show up overnight. It can take days or even weeks for enzyme levels to rise—or fall—after you change your routine. That’s why some people feel fine at first, then suddenly get sick or their condition worsens. It’s not a coincidence. It’s pharmacokinetics in action. And if you’ve ever wondered why your painkiller stopped working after you started taking a new supplement, or why your cholesterol shot up after switching antibiotics, CYP3A4 induction might be the hidden reason.
Some of the posts below dive into how this plays out in real life. You’ll find stories about how generic drugs interact with enzyme activity, how timing your pills can avoid dangerous drops in drug levels, and how the FDA tracks these hidden risks after approval. You’ll see how dose splitting, food interactions, and even gut health can tie into this same system. This isn’t just about one enzyme. It’s about how your whole body handles medication—and how easily things can go wrong if you don’t know what to watch for.
Rifampin is essential for treating tuberculosis but causes dangerous drug interactions by boosting liver enzymes. Learn how it affects birth control, blood thinners, HIV meds, and more-and what you can do to stay safe.