Generic vs Brand Medications: What Really Matters for Your Health
When you pick up a prescription, you might see two options: the generic drug, a medication with the same active ingredient as a brand-name drug, approved by regulators to work the same way. Also known as generic equivalent, it often costs far less but does the same job. Or you might get the brand-name drug, the original version developed by a pharmaceutical company, often protected by patents and sold under a trademark. Also known as originator drug, it’s the one you see advertised on TV. The big question isn’t which is better—it’s whether you’re getting the same result. The answer, backed by real-world science, is usually yes.
Here’s how it works: before a generic drug hits the shelf, it must prove it’s bioequivalent, a technical term meaning it delivers the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. Also known as pharmacokinetic match, it’s measured using two key numbers—Cmax and AUC. These aren’t marketing buzzwords—they’re lab-tested metrics. If a generic drug’s peak concentration (Cmax) and total exposure (AUC) fall within strict limits compared to the brand, regulators approve it. That’s not guesswork. That’s science. And it’s why millions of people safely use generics every day—from blood pressure pills to antidepressants.
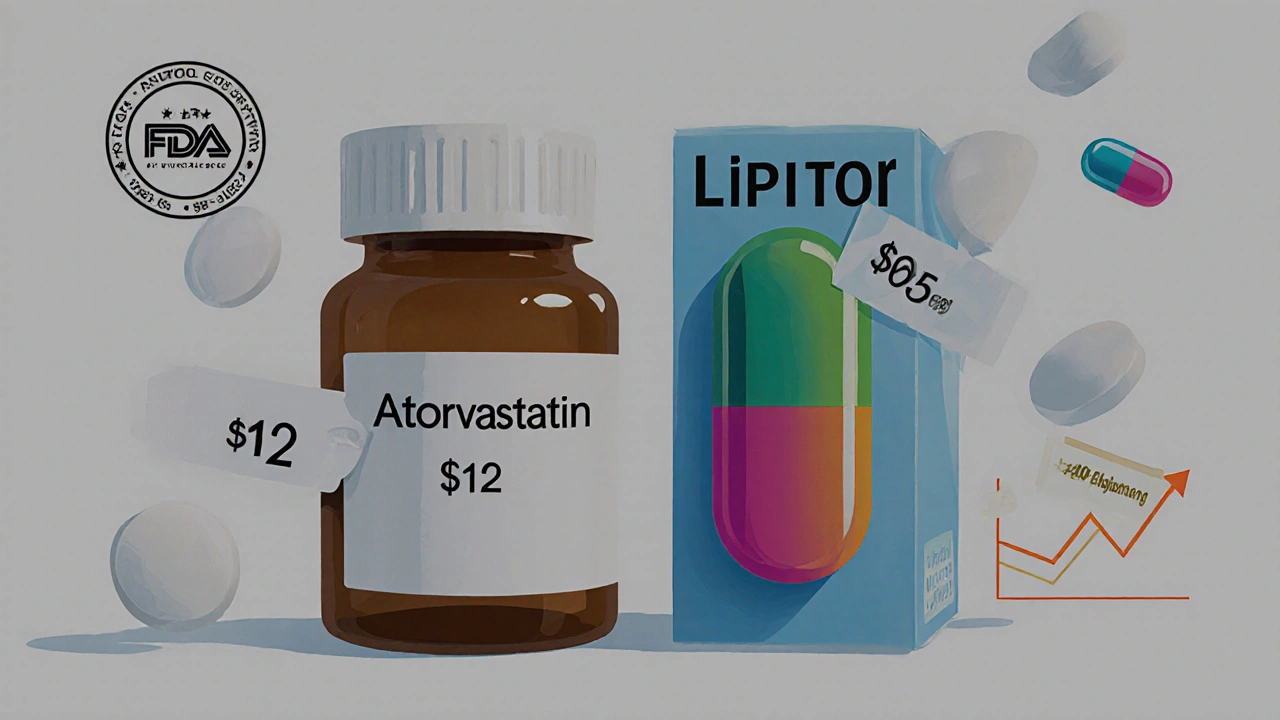
So why do brand-name drugs cost so much more? Mostly because of patents. When a company invents a new drug, they get years of exclusive rights to sell it. Once that expires, other manufacturers can make the same medicine without repeating expensive clinical trials. The savings get passed on. A generic version of Zoloft might cost $10 instead of $150. That’s not a trick. That’s how the system’s supposed to work.
Some people worry about inactive ingredients—fillers, dyes, or coatings. These don’t affect how the drug works in your body. But if you’re allergic to a specific dye or have trouble swallowing a large pill, those details matter. That’s when talking to your pharmacist helps. Most generics are identical in effect, but a few might look or taste different. That’s okay. What matters is whether it lowers your blood sugar, fights infection, or eases anxiety—and it almost always does.
There’s one exception: drugs with a narrow therapeutic index. These are tricky. Too little doesn’t work. Too much causes harm. For these, like warfarin or thyroid meds, your doctor might prefer you stick with one version—brand or generic—to avoid tiny shifts in how your body responds. But even then, switching isn’t dangerous if done under supervision.
What you’ll find in the posts below isn’t theory. It’s real-world proof. We’ve got side-by-side comparisons of generic vs brand antibiotics, cost breakdowns for popular meds like Accutane and Zyrtec, and deep dives into how regulators verify equivalence. You’ll see how people manage medication costs during travel, what to watch for when switching, and why some doctors still push brand names—not because generics don’t work, but because habits die hard.
Generic medications save patients and insurers billions by offering the same effectiveness as brand-name drugs at a fraction of the cost. Learn why generics cost less, how to find the best prices, and when to question high-cost alternatives.
Generic drugs save Americans billions annually and are just as effective as brand-name versions. Learn the key differences, safety facts, cost savings, and when to stick with brand-name meds.