Tuberculosis Treatment: What Works, What to Watch For
When it comes to tuberculosis treatment, a multi-drug regimen designed to kill Mycobacterium tuberculosis bacteria over months, not days. Also known as anti-TB therapy, it's one of the most time-intensive but critical drug courses in modern medicine. Unlike a simple infection you can clear in a week, TB demands patience, precision, and persistence. Skip a dose? Delay a refill? You’re not just risking your own health—you’re helping create drug-resistant strains that can spread to others.
Most cases start with a four-drug combo: isoniazid, rifampin, ethambutol, and pyrazinamide. These aren’t optional extras—they’re the backbone. After the first two months, you usually drop two of them and keep going with just isoniazid and rifampin for another four to seven months. That’s six to nine months of daily pills. No shortcuts. The TB antibiotics, the specific drugs used to kill tuberculosis bacteria, often requiring long-term use and strict monitoring work slowly because TB bacteria hide deep in lung tissue and multiply at a crawl. That’s why treatment lasts so long: you have to kill every last one, or they come back stronger.
And then there’s the problem of drug-resistant TB, a form of tuberculosis that doesn’t respond to standard first-line antibiotics, requiring longer, more toxic regimens. If you’ve had TB before and didn’t finish your meds, or if you live in a region with poor access to care, you might be dealing with resistant strains. That means switching to second-line drugs like bedaquiline or linezolid—drugs with more side effects, higher cost, and longer treatment times (up to 18–24 months). It’s not just harder—it’s heavier on your body. Liver damage, nerve issues, hearing loss: these aren’t rare. That’s why regular blood tests and doctor visits aren’t optional. They’re survival tools.
What about side effects? Nausea, fatigue, orange urine (thanks, rifampin), and tingling hands? They’re common. But they’re not always a reason to quit. Many people push through with support from their clinic or pharmacist. If you’re struggling, talk to your provider before stopping. There are ways to adjust timing, manage symptoms, or even switch drugs—without letting the TB win.
This collection of articles doesn’t cover every TB drug in detail—but it does show you how medication safety, timing, and monitoring apply directly to long-term treatments like this. You’ll find real insights on how to avoid dangerous interactions, why splitting doses doesn’t work here, how to track recalls on your meds, and what to do when side effects pile up. It’s not about guessing. It’s about knowing exactly what your body’s going through—and how to stay in control.
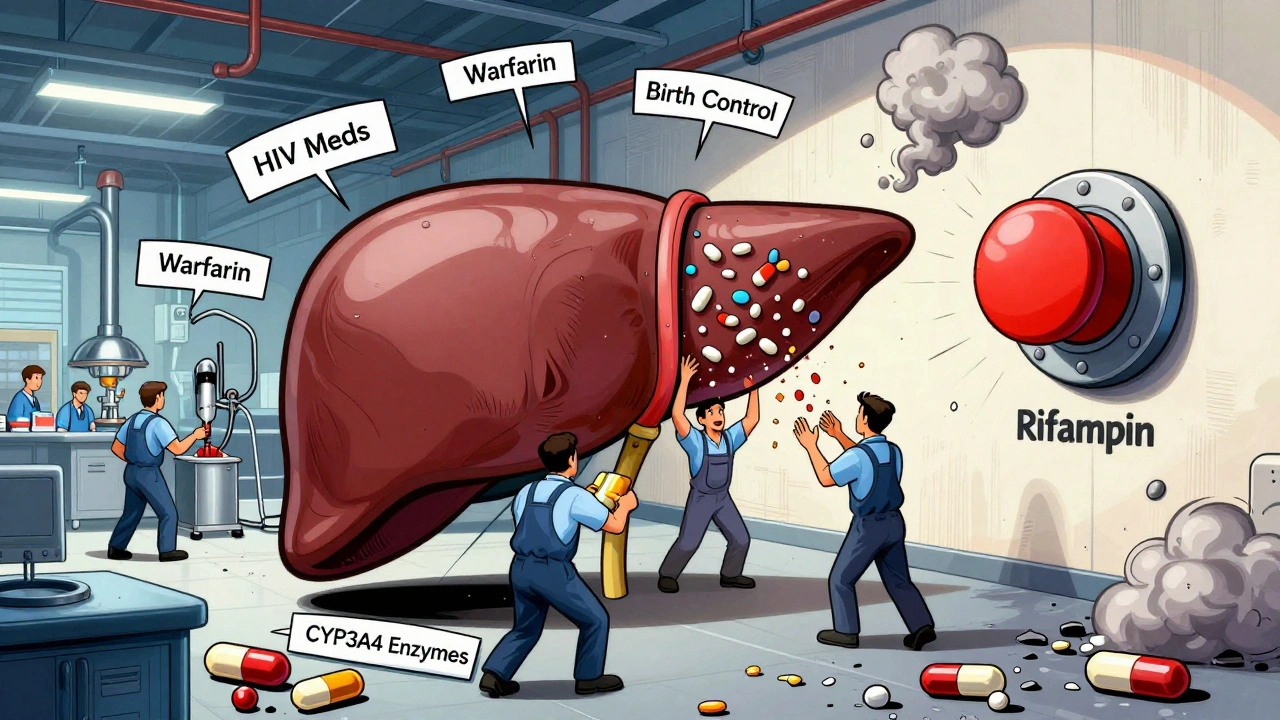
Rifampin is essential for treating tuberculosis but causes dangerous drug interactions by boosting liver enzymes. Learn how it affects birth control, blood thinners, HIV meds, and more-and what you can do to stay safe.